Effect of myofascial release and muscle energy technique on patients with chronic neck pain: a scoping review
Article information
Abstract
[Purpose]
To identify the effects of muscle energy techniques and myofascial release in patients with chronic neck pain.
[Methods]
To conduct a literature search and identification; PRISMA-ScR guidelines were followed. Relevant articles were searched for from the following medical and health sciences electronic databases: PubMed, EBSCOhost, CENTRAL of the Cochrane Library, and the Physiotherapy Evidence-Based Database (PEDro). Patients with chronic neck pain were eligible for the scoping review.
[Results]
Seven articles were included in this review. This scoping review found that there is heterogeneity in the prescription of MFR and MET and a greater tendency to check three major physical dimensions (pain, range of motion, and disability). Various studies have opted for distinct intervention regimens, resulting in disparities in the frequency of weekly interventions, which can range from biweekly to five times a week. These inconsistencies may lead to perplexity among practitioners, as each intervention modality demonstrates favorable outcomes for individuals with persistent cervical discomfort. Moreover, a significant proportion of research projects have employed the numeric pain rating scale (NPRS) and visual analog scale (VAS) for data quantification.
[Conclusion]
According to results, majority of the studies were focused on pain and missing components of range of motion and quality of life. Work-related factors can act as risk factors for chronic neck pain. Future investigations should adopt a comprehensive methodology and incorporate QoL assessments of quality of life.
INTRODUCTION
Neck pain is the fourth most common cause of disability worldwide. The definition of cervical spinal pain, as outlined by the International Association for the Study of Pain (IASP) in its classification of Chronic Pain, refers to “pain experienced in any location within the posterior area of the cervical spine, ranging from the superior nuchal line to the first thoracic spinous process.” The adult population aged 15–74 years exhibited a point prevalence ranging from 5.9% to 38.7%. The prevalence of neck pain in the elderly population for a duration of one year varied between 8.8% and 11.6%. Females exhibit a higher frequency of reported neck pain in comparison to males [1]. Due to disrupted thickness, altered cross-sectional area may cause chronic neck pain among adults. Due to the propensity for cervical discomfort to manifest as a persistent concern, it is imperative to discern the determinants that may foster the implementation of preventive measures and prompt identification at an early stage [2,3].
Neck pain is a complex condition with various contributing factors. Many studies conducted in the general population have focused on the impact of different modifiable and non-modifiable elements on the occurrence of neck pain. These factors include, but are not limited to, advanced age, female sex, inadequate social support, and a history of neck or lower back pain. Given the proclivity of neck pain to evolve into a persistent issue, the identification of risk factors is of paramount importance for facilitating preventive measures and early detection [3,4]. The etiology of neck pain is multifaceted, and a plethora of factors can potentially influence its onset. Nevertheless, there is a strong body of evidence supporting certain risk elements, such as a sedentary lifestyle, prolonged daily screen time, perceived psychological stress, and female sex. By identifying protective and risk factors, triggers, and potential outcomes, strategies can be developed to prevent, diagnose, treat, and manage neck pain [5].
Myofascial release (MFR) [4] and muscle energy techniques (METs) [5] are useful non-invasive, non-pharmacological techniques that provide symptomatic relief in patients with chronic neck pain. Previous studies have shown positive improvements in trapezius and suboccipital muscle tenderness after the application of MFR. One randomized controlled trial identified MET as a beneficial treatment approach for improving pain, disability, and neck range of motions (physical dimensions). Despite the extensive use of physiotherapy and alternative conservative therapeutic methodologies, there is insufficient literature containing superior research substantiating the application of these treatment techniques. We aimed to identify the benefits of MFR and MET for the treatment of chronic neck pain, which is currently characterized as a social burden.
According to the available literature, there is a definite need to identify the appropriate methods, benefits, and medical concerns associated with these therapeutic approaches. This scoping review will identify the potential reasons of choosing MFR and MET for the treatment of chronic neck pain using Arksey O’ Malley and Levac et. al guidelines [6]. Research question: Is there any research showing the benefits of MFR and MET for the treatment of patients with chronic neck pain?
METHODS
A scoping review was undertaken due to the exploratory nature of the research query. Scoping reviews have proven beneficial for delineating fundamental ideas, categories of evidence, and research deficiencies within a specific domain. They examine the extent, scope, and essence of evidence concerning a particular subject or query; ascertain the worth of embarking on a methodological review; and strategize forthcoming investigations [7].
Search strategies
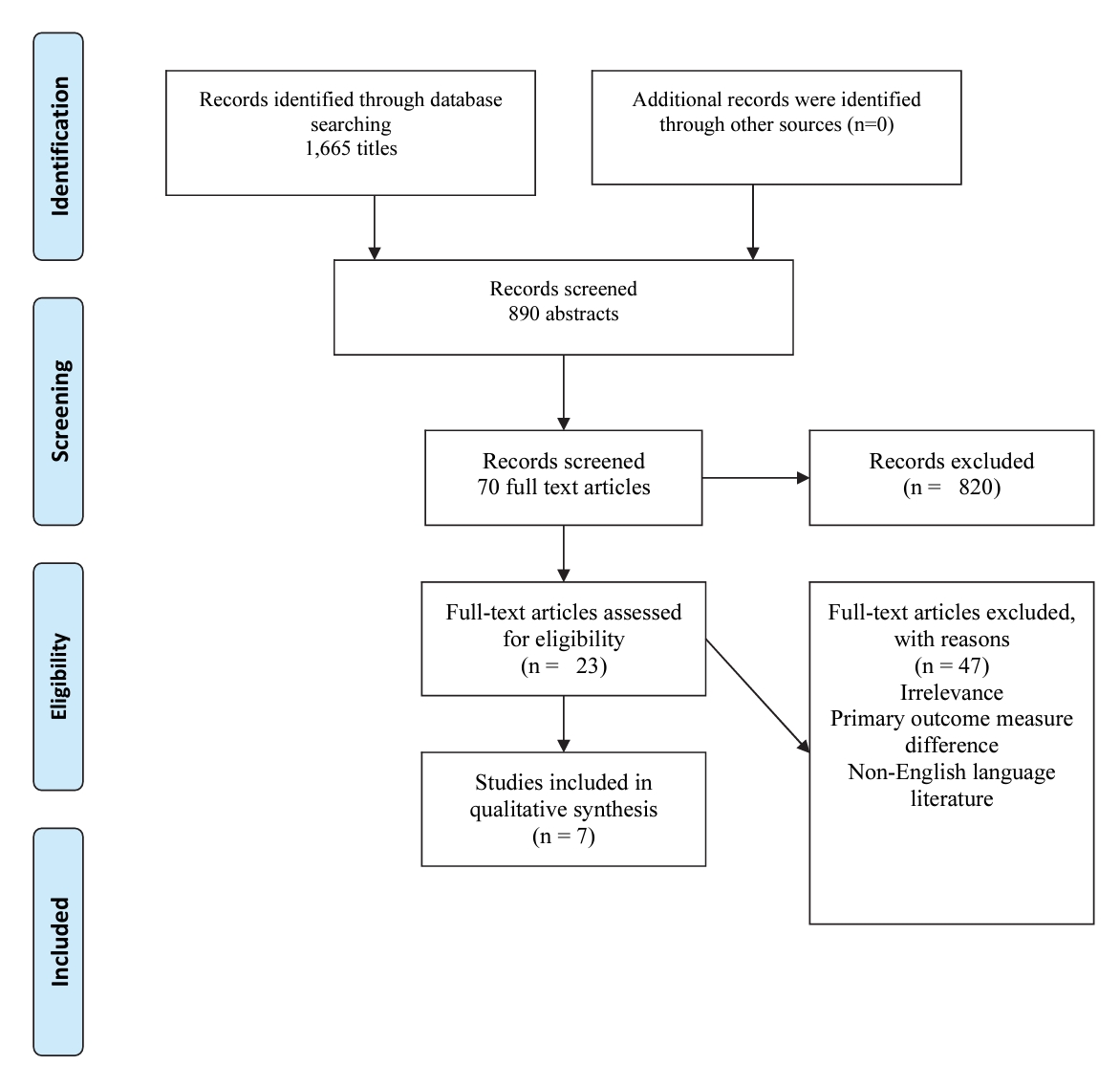
To conduct the literature search and identification, PRISMA-ScR guidelines were followed [8]. Relevant articles were searched from following medical and health sciences electronic databases: PubMed, EBSCOhost, CENTRAL of Cochrane Library, and Physiotherapy Evidence-Based Database (PEDro). Key terms used for systemic search were, “Myofascial” AND “Muscl* Release” AND “Musc* OR “Muscle” AND “Neck” AND “Neck Pain” AND “Chronic” AND “Muscle energy technique” AND “Energy technique” AND “MET” AND “MFR. “These keywords were helpful in identifying titles, abstracts, and full-text articles for inclusion in the scoping reviews. The keywords included were based on three main concepts: myofascial release, muscle energy technique, and Chronic Neck pain. The search terms used are listed in Table 1.
The subsequent phase entailed a thorough examination of the electronic databases to detect conceivably pertinent articles that had been published until April 25, 2020, without any restrictions imposed on the date of publication. The search for articles was completed on January 20th, 2024, by both authors. Subsequent to the selection of articles, a retrospective tracing procedure was undertaken on the reference lists of the aforementioned articles that had been included, to identify articles that had the potential to be deemed eligible.
Eligibility criteria
In this scoping review, eligibility criteria were based on the PICOS (participants, intervention, comparator, outcomes, and study design) guidelines. The study characteristics are presented in Table 2.
Evidence selection
The initial evaluation was conducted by two independent evaluators who examined the titles and abstracts to evaluate their potential suitability, excluding those that clearly did not meet the inclusion criteria. Articles from different databases were checked using the SM. Repetition of articles resulted in the authors selecting only one database. Other studies were excluded to avoid reproducibility. All articles were imported into the Mendeley reference management software, and duplicates were excluded. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart was used to direct the selection and evaluation processes. At this stage, a more comprehensive approach was adopted, opting not to exclude uncertain articles, thereby increasing the likelihood of including all potentially relevant studies. The second evaluation phase was conducted by the same two independent evaluators who thoroughly read the complete text of the included articles. The focus shifted towards greater precision, selecting only articles that fully satisfied the eligibility criteria. In instances of uncertainty, a third reviewer was consulted to determine the eligibility for inclusion.
Process of data charting
Two reviewers independently extracted data for various categories, including authorship, publication year, study design, MFR and MET protocols, rehabilitation time frame, study population, sample characteristics (e.g., size, sex, and average age), rehabilitation outcomes, and specific training parameters (such as exercises, sets, repetitions, and frequency).
Critical appraisal tool
One evaluator used the OCEBM LoE framework developed by the Oxford Center for Evidence-Based Medicine to appraise each article. The OCEBM LoE framework serves as a concise and efficacious instrument for assessing the robustness of findings in research studies and determining the methodological soundness of each article [9]. In accordance with this particular system, the articles were categorized based on their LoE, ranging from level I (indicating a higher LoE) to level V (indicating a lower LoE). A higher LoE indicates superior methodological quality and reduced likelihood of bias.
RESULTS
Evidence selection
The literature search yielded 70 articles. After removing duplicates, 23 articles were screened based on titles and abstracts. Seven full-text articles were identified based on eligibility criteria. Information on the included articles is summarized in the PRISM-ScR flow diagram. The general characteristics of the included studies are presented in Table 3.
Results synthesis
Level of evidence and study designs
Based on the methodological designs of the eight included articles, six were randomized controlled trials (RCTs) [1,10-14] and one [15] study was a pre-post test quasi-experimental study. This scoping review included seven randomized controlled trials (RCTs) with LOE II according to the OCEBM LoE framework.
Sample characteristics
This scoping review identified available studies showing the benefits of MFR and MET for the treatment of 514 patients with chronic neck pain. In three studies, the percentages of males and females were not identified by the authors. In the other five articles, 199 were female and 108 were male.
Protocol characteristics
Most studies compared interventions (MET and MFR) with other treatments. Two studies compared the effects of post-isometric relaxation, instrument-assisted soft tissue mobilization, and MFR. One study compared the effects of facet joint mobilization with those of the MET and MET alone in four studies.
Outcomes used to find treatment efficacy
All seven studies used the visual analog scale (VAS) to identify the severity of pain and the neck disability index (NDI) to identify the disability index among patients with neck pain. In four studies, a universal goniometer was used to check the cervical range of motion. In two studies, a pressure algometer was used to check the pain pressure threshold. In one study, the WHO-BREF-QOL-100 was used to assess the patients’ quality of life.
DISCUSSION
This scoping review identified seven articles that compared the effects of MFR and MET to those of other treatments. The primary purpose of this scoping review was to determine the efficacy of MFR and MET, which demonstrates the lack of published literature on these treatments in patients with chronic neck pain.
Studies showing how muscles adapt to the physical function of individuals after administering these interventions are scarce. Furthermore, this scoping review found that there is heterogeneity in the prescription of MFR and MET and a greater tendency to check three major physical dimensions (pain, range of motion, and disability). Each study selected different sets for the interventions, ranging from 3 to 10 repetitions. There was also a discrepancy in weekly interventions, which ranged from twice to five times a week. The height of each muscle varied between 10 and 30 s. These discrepancies can cause confusion among healthcare providers, because each treatment method yields positive results in patients with chronic neck pain. Furthermore, a notable number of studies have utilized the NPRS and VAS to quantify data [15,16]. There might exist Several factors may have contributed to the heterogeneity across studies. One prominent factor identified was the disparity in pain assessments among individuals suffering from chronic neck pain [17]. For instance, in the investigation by Shewail et al., the Visual Analog Scale (VAS) recorded a mean score of 3.40 ± 1.12, whereas Tabassum H et al. reported a pain range of 7 ± 1. Hence, variations in pain scores could potentially influence treatment dosage. Another factor that contributed to heterogeneity was the use of diverse outcome measures. The use of different outcome measures has the potential to introduce bias within the same study population.
Post isometric relaxation (PIR) versus MFR
One study showed that PIR and MFR are efficacious in mitigating nonspecific neck pain. Nevertheless, individuals with nonspecific neck pain who underwent PIR displayed an overall superior outcome when considering the visual analog scale VAS, cervical extension and rotation, NDI, and World Health Organization Quality of Life BREF 100 (social domain) in comparison to those who received myofascial release therapy (MFR) after a duration of 2 weeks [18].
Instrument assisted soft tissue manipulation (IASTM) versus MFR
In another study comparing IASTM and MFR, the effects of IASTM and MFR techniques seemed to be comparable in terms of the pain and disability experienced by college students engaged in distance learning and suffering from chronic neck pain. Nonetheless, individuals who underwent IASTM treatment exhibited modest yet discernible improvements in pain, functionality, and pain pressure threshold [10].
MET and facet joint mobilization (FJM)
were determined to be efficacious in reducing neck pain and disability by means of enhanced cervical range of motions in comparison to traditional physiotherapy, with the exception of cervical lordosis and extension ROM, in which FJM surpassed both groups, according to Tabassum et al.. Although the MET surpassed the FJM in terms of flexion, rotation, and side bending in both directions, there was no notable discrepancy between the FJM and MET with respect to pain intensity and functional disability [11].
MET versus Ischemic compression technique
One study demonstrated that the combination of MET and ICT was more effective than MET alone in reducing neck pain and muscle tenderness in male patients with upper trapezius active myofascial trigger points (MTrPs). The immediate and short-term effects of this combination therapy have established it as a primary treatment plan in the clinical setting for addressing neck pain and muscle tenderness caused by active (MTrPs) [12]. The clinical significance of our findings is that MET plus ICT is highly efficient in alleviating MTrP pain within a brief timeframe. Moreover, this treatment approach is cost-effective and can be implemented in clinical settings.
Comparative effects of autogenic inhibition and reciprocal inhibition
A study comparing autogenic inhibition and Reciprocal Inhibition of the MET concluded that autogenic inhibition (AI-MET) is more advantageous than reciprocal inhibition (RI-MET) in enhancing pain, Range of Motion, and functional disability among individuals with subacute and chronic MNP. AI-MET has demonstrated noteworthy enhancements in terms of immediate and long-term effects on MNP across all evaluative criteria [13]. Consequently, it a feasible technique to combine with conventional neck pain therapy to achieve superior treatment outcomes for individuals with MNP.
Limitations
There were a few limitations to the included studies. One significant drawback is the lack of comprehensive assessment of the results over an extended period. Additional research using larger follow-up durations and control groups is necessary to ascertain the extended clinical advantages and apply the intervention findings to a broader population. The aforementioned studies demonstrated the beneficial effects of MFR and MET on individuals with chronic neck pain; however, they neglected to address potential publication biases. In future investigations, it is advisable to restrict the inclusion of studies that highlight specific advantages and variables over substantial outcomes. Another constraint is the limited scope of the search strategy. Broadening the search approach can augment the number of articles incorporated into the analysis and improve the comprehensiveness of the methodology. The assessment provided may not accurately depict the effectiveness of treatments (MFR and MET) that have been documented in languages other than English, because studies in non-English languages were not included. While gray literature, such as conference abstracts, was also excluded, it is improbable that they contained the necessary data for research evaluation owing to limitations in word count.
This review had several strengths. We conducted a thorough exploration of studies published between January 2012 and December 2022 across five electronic databases, encompassing a diverse array of studies examining all facets of musculoskeletal concerns among students. Moreover, to ensure agreement among the reviewers, we established a robust methodology and evaluation that considers the OCEBM LoE framework reporting criteria.
Future implications
In future research, it will be necessary to shift the emphasis towards examining quality of life and various work-related elements that contribute to the development of chronic neck pain. Previous research has predominantly focused on exploring the correlations between specific risk factors and neck pain as opposed to conducting a comprehensive analysis that encompasses both individual and work-related variables.
CONCLUSION
Our primary aim was to assess the breadth of research conducted in this specific field, owing to the increasing importance attributed to musculoskeletal complications. Subsequently, we encountered a wide-ranging array of evidence that substantiated the efficiency of several treatment modalities, a phenomenon frequently recorded in scholarly studies employing a multitude of parameters across varying temporal scopes. It is advisable that future inquiries embrace an exhaustive approach in their methodology and include evaluations pertaining to quality of life.