Effect of blood flow restriction with low-intensity resistance training in patients with osteoarthritis and rheumatoid arthritis: a systematic review and meta-analysis based on randomized controlled trials
Article information
Abstract
[Purpose]
This study evaluated the effects of blood flow restriction with low-intensity resistance training (BFR + LIRT) on pain, adverse events, muscle strength, and function in patients with osteoarthritis (OA) and rheumatoid arthritis (RA) through a systematic review and meta-analysis.
[Methods]
This study adhered to the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analyses 2020 (PRISMA 2020) and applied the A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR2) standards to ensure the high quality of the systematic review. A comprehensive literature search was conducted until August 2023 using four selected keywords (osteoarthritis, rheumatoid arthritis, blood flow restriction training, and resistance training) across five search engines (PubMed, Embase, Web of Science, CENTRAL, and PEDro).
[Results]
Ten studies were analyzed. The results showed that BFR + LIRT had similar effects on pain, risk of adverse events, muscle strength, self-reported function, and physical function compared with resistance training (RT).
[Conclusion]
This systematic review and meta-analysis further support the potential of BFR + LIRT in the disease management of patients with OA or RA. According to this analysis, BFR + LIRT had a lower risk of adverse events than high-intensity resistance training (HIRT) and may be a safer training modality. BFR + LIRT offers greater advantages in improving physical function than LIRT and was able to provide similar benefits to HIRT without increasing the training load. These findings suggest that BFR + LIRT is a safe and effective strategy for treating patients with OA or RA. However, owing to the limited number of studies covered in this analysis, additional higher-quality studies are needed to strengthen this conclusion.
INTRODUCTION
Arthritis is a common chronic disease and one of the leading causes of human disability worldwide [1]. Among these, osteoarthritis (OA) and rheumatoid arthritis (RA) are the most common types, with estimated global populations of approximately 528 million and 18 million patients, respectively [2]. OA is a musculoskeletal disorder primarily attributed to the degeneration or injury of the joint cartilage, characterized pathologically by cartilage deterioration, structural alterations, and mild-to-moderate synovial inflammation [3]. RA, on the other hand, is classified as an autoimmune disease, characterized by abnormal activation of the immune system, resulting in synovial inflammation, cartilage destruction, and bone damage [4]. Despite the different pathomechanisms, the clinical symptoms of the two diseases are similar, including joint pain, stiffness, swelling, muscle atrophy, and limited mobility, which can seriously affect the quality of life. Age is a major risk factor for OA and RA [3,4]. As life expectancy increases globally and the population ages, the prevalence and number of patients with these two diseases are gradually increasing [5-7]. Therefore, addressing the impact of these diseases on the global health and healthcare systems is an urgent issue.
At present, the management goals for OA and RA are focused on improving joint pain, muscle atrophy, and functional limitations, as well as mitigating potential adverse events or side effects [8]. The World Health Organization recommends muscle-strengthening exercises as a rehabilitation management strategy to improve pain and function in patients with these diseases. Resistance training (RT) is a popular form of muscle-strengthening training [9]. This common form of exercise aims to increase muscle mass, strength, and anaerobic endurance by overcoming the resistance provided by skeletal muscles [10]. Given the prevalence of muscle atrophy in OA and RA patients, the strategic addition of high-intensity resistance training (HIRT) has emerged as an effective strategy to address these challenges [11,12]. However, high-load training is more prone to further joint injury because of the common occurrence of pain and functional impairment in joints affected by OA and RA [13,14]. In addition, inappropriate or overly vigorous training regimens can reduce patient adherence, increase discomfort and pain, and jeopardize health.
Blood flow restriction with low-intensity resistance training (BFR + LIRT) has been a highly favored training modality in recent years with the potential to improve muscle strength and mass. During LIRT, BFR intervention is used to limit the inflow and outflow of blood by applying a blood pressure cuff of a specific width and pressure around the contracting muscle, exposing the muscle to ischemia and hypoxia, stimulating growth hormone secretion, increasing lactic acid concentration, enhancing satellite cell activity, and promoting the growth of more muscle fibers, thereby enhancing muscle strength and contraction of muscle hypertrophy [15]. This effect, which leads to increased muscle strength and hypertrophy, is similar to implementing HIRT [15,33,37]. Therefore, high-load training may be inappropriate or intolerable in patients with OA or RA. High-load training is often associated with pain and adverse events [34]. Therefore, the smaller training load of BFR + LIRT helps alleviate pressure and stress on the joints and soft tissues, reducing the potential risk of injury and occurrence of adverse events [16]. In addition, the implementation BFR + LIRT elevates endorphin levels, reduces pain perception, and elevates pain thresholds [17]. These characteristics warrant attention in the clinical management of patients with musculoskeletal disorders.
Recently, increasing attention has been paid to the role of BFR + LIRT in the clinical management of OA and RA. Despite growing awareness, their clinical use remains relatively limited. To date, only one study has systematically assessed muscle strength, muscle mass, and function in these patients; however, that study had several limitations [18]. Although muscle strength, mass, and function are critical in disease management, the implementation of safe and painfree clinical treatment programs is equally important [19]. The impact of pain and adverse events during clinical rehabilitation is also concerning. In addition, this systematic evaluation and meta-analysis may have led to discrepancies in the results owing to limited study sample sizes. Therefore, the inclusion of more randomized controlled trials might have resulted in more accurate meta-analyses. In summary, this systematic evaluation and meta-analysis aimed to assess the effects of BFR + LIRT on pain, adverse events, muscle strength, and function in patients with OA and RA and to provide valuable recommendations for the management of rehabilitation in patients with these diseases.
METHODS
Study design
This study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) guidelines and complied with the standards of A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR2) for conducting high-quality systematic reviews [20,21]. The research protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO; CRD: 42023339448).
Search strategy
Six electronic databases, MEDLINE (via PubMed), Embase, Web of Science, Scopus, PEDro, and CENTRAL, were searched through November 2023. The keywords used were “osteoarthritis,” “rheumatoid arthritis,” “blood flow restriction training,” and “resistance training.” Relevant Medical Subject Headings (MeSH) and terms for each keyword were obtained from the National Library of Medicine. All synonyms were concatenated with “OR” and parts were concatenated with “AND” to construct the search string. In addition, a manual search of Google Scholar was conducted to verify the results of other databases. The search was limited to full-text articles in English, with no restrictions on the publication date.
Inclusion/exclusion criteria
Inclusion criteria
To identify eligible studies, we used the PICO framework to develop eligibility criteria, as follows: (i) Participants: studies that included individuals at risk or with a diagnosis of OA or RA; (ii) Intervention: studies that provided BFR + LIRT intervention; (iii) Comparison: studies that compared BFR + LIRT with HIRT (≥60% 1RM) or LIRT (<60% 1RM); (iv) Outcomes: studies that reported pain, adverse events, muscle strength, self-reported function, and physical function outcomes.
Exclusion criteria
The following exclusion criteria were used: (i) studies that included participants with any musculoskeletal diseases other than OA or RA were excluded; (ii) studies that involved acute effects (intervention duration ≤2 weeks) were excluded; (iii) studies that included participants who received other management measures in addition to the intervention were excluded; (iv) studies that were of the following types were excluded: reviews, case reports, conference abstracts, observational studies, letters, studies that reported results that had been previously reported, and incomplete studies.
Studies that met all the eligibility criteria were included. Studies meeting any of the exclusion criteria were excluded. Studies that could not be assessed for eligibility or those that were excluded based on the title and abstract were reviewed to determine eligibility.
Data extraction
After screening for duplicate studies and eligibility, data were extracted for eligible studies. The extracted data included the following authors, year of publication, participant characteristics (number, age, sex, and disease), intervention characteristics (cuff size, cuff pressure, intervention type, intervention load, intervention duration, and frequency), and outcome measures (pain, adverse events, muscle strength, self-reported function, and physical function). For data that were not clearly reported, we contacted the corresponding authors to obtain the data. If we did not receive a response, we extracted the data using GetData Graph Digitizer software (version 2.24, GetData Pty Ltd., NSW, AUS) or computed the data following the procedures outlined in the Cochrane Intervention System Review Handbook [22]. In instances where data provision was not feasible, data were not quantitatively analyzed and only qualitative synthesis was conducted.
Primary and secondary outcomes
Given the limitations of previous studies, the primary outcome of this study was pain and adverse events. Pain relief was assessed using participant-reported subjective pain rating scales encompassing multiple pain assessment tools. We employed the internal consistency coefficient (Cronbach’s alpha) and test-retest reliability coefficient (intraclass correlation coefficient, ICC) to evaluate the reliability of the pain assessment scales. Specifically, the reliability of pain assessment scales for OA or RA is as follows: the Visual Analog Scale (VAS) has an ICC of 0.97 [23]. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) achieved a Cronbach’s alpha of 0.82 [24]. The Knee Injury and Osteoarthritis Outcome Score (KOOS) exhibits a Cronbach’s alpha of 0.916 [25]. The Numeric Pain Rating Scale (NPRS) records an ICC of 0.95 [23]. These scales have consistently shown high reliability for pain detection. Regarding adverse event outcomes, clearly reported adverse events related to or caused by the intervention, including pain, discomfort, and inability to undergo the training program, were included and extracted.
The secondary outcome of this study was to evaluate the impact of BFR + LIRT compared to RT on muscle strength, self-reported function, and physical function in patients with OA and RA. Muscle strength outcomes were assessed by measuring quadriceps muscle strength using single-joint knee extension and multijoint leg press tests. Self-reported functional results were evaluated using subjective function rating scales. Outcomes related to physical function were assessed using timed up-and-go (TUG) and timed stair climb (TST) tests.
Methodological quality assessment
The methodological quality of the present study was assessed using the Physiotherapy Evidence Database (PEDro) scale, which comprises 11 assessment elements: random allocation, concealed allocation, baseline comparability, blind subjects, blind therapists, blind assessors, adequate follow-up, intention-to-treat analysis, between-group comparisons, point estimates and variability, and eligibility criteria. The eligibility criteria were not included in the total score calculations. For the remaining assessment elements, each received one point when met and none when not met, with a maximum total score of 10. The total score was then categorized into specific ranges: 0-3 as “poor,” 4-5 as “fair,” 6-8 as “good,” and 9-10 as “excellent” [26].
Risk of bias assessment
The risk of bias in the randomized controlled trials was assessed using the Risk of Bias in Randomized Clinical Trials tool 2.0 (RoB2.0) from the Cochrane Collaboration. RoB2 is a reliable tool for detecting the risk of bias in randomized controlled trials (RCTs) studies. The randomization process, deviations from intended interventions, missing outcome data, outcome measurements, and selection of reported results were examined. These questions were rated in five levels: Y (Yes), PY (Probably Yes), NI (No Information), PN (Probably No), and N (No). Finally, the questions were summarized and classified as having a low risk of bias, some concerns, or a high risk of bias [27].
Statistical analysis
We performed the meta-analysis using STATA 17 software (StataCorp, College Station, TX, USA). To calculate effect sizes (ES) for the continuous variables of pain, muscle strength, and function, the Hedges g method was used to calculate the standardized mean difference (SMD) and its corresponding 95% confidence interval (95% CI) [28]. To calculate the ES for the dichotomous variables of adverse events, we used the log risk ratio (log RR) and its corresponding 95% CI. Statistical significance was judged based on the location of the upper and lower limits of the 95% CI, which were considered statistically significant if they were on the same side of the line of no effect; conversely, they were not statistically significant if they intersected the line of no effect. The level of heterogeneity was categorized as low (25%), medium (50%), or high (75%), based on the I² statistic [29]. In selecting the effect model, if I² ≥50%, a random effect model with Hedges was used; otherwise, a fixed effect model with inverse variance was used. To explore the stability of the meta-analysis results and sources of study heterogeneity, we conducted a rejection of cross-validation (LOOCV) sensitivity analysis to systematically exclude individual studies and observe their impact on the overall effect size. If the exclusion of a study resulted in a significant change in the effect size, it was considered the main factor contributing to the high between-study heterogeneity, whereas if the exclusion of a study did not result in a significant change in the effect size, this indicated a high level of reliability of the meta-analysis results. In addition, we conducted subgroup analyses according to intervention load, disease type, and sex.
RESULTS
Search results
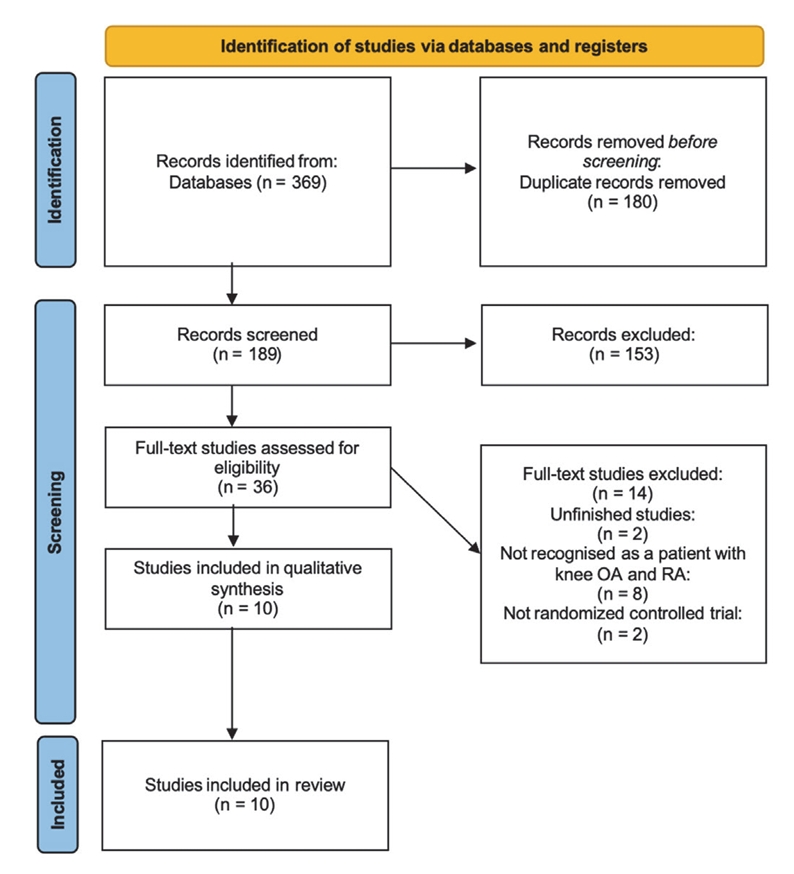
Using our search strategy, 369 relevant citations were found in five electronic databases. After performing a duplicate review using reference management software, 180 duplicate citations were removed. Of the remaining 189 unique citations, 153 articles were excluded based on the eligibility and exclusion criteria, leaving 36 articles. A full-text review was then conducted to evaluate the remaining articles. The full text of 26 articles were found and excluded as not meeting the eligibility criteria. The remaining ten studies were included in the systematic review and meta-analysis. The PRISMA flowchart is presented in Figure 1.
Characteristics of studies
All of the included studies were RCTs and were published between 2015 and 2023.
Participants
A total of 350 participants were included in the 10 studies. The mean age of the participants ranged from 45 to 69 years. Regarding the disease characteristics of the participants, eight studies involved individuals with OA [30-35,38,39], and two studies involved individuals with RA [36,37]. In terms of the sex distribution, six studies included female participants [31-33,35-37], one study included male participants [30], and three studies included both sexes [34,38,39]. Table 1 provides further details on the characteristics of the study participants.
Occlusion
The cuff position was fixed at the lateral third of the thigh muscle in all the included studies. Subsequently, two studies by Segal et al. used gradual incremental pressures ranging from 160 to 200 mmHg [30,31]. Both studies reported a fixed cuff pressure of 50 mmHg [38,39] and a 70% relative percentage limb occlusion pressure (LOP) [33,37]. Two studies used a fixed pressure of 200 mmHg [32,35]. One study used 50% arterial occlusion pressure (AOP) to control the flow restriction [36]. Harper et al. used an individualized pressure formula to determine unique cuff pressures [34]. Regarding cuff size, four studies used cuffs that were >17 cm wide [33,37-39], four studies used cuffs that were only 5-7 cm wide [30,31,35,36], and two studies did not report the size of the cuffs used [32,34].
Intervention
For the intervention group training load (BFR + LIRT group), all but one study used BFR combined with 20-30% 1RM LIRT [30-35,37-39]. Jonsson et al. reported using BFR combined with 30-50% 1RM LIRT [36]. For training loads in the control group, six studies used LIRT [30,31,33,36,38,39] and five studies used HIRT [32-35,37]. Notably, Ferraz et al. used 70% 1RM HIRT and 30% 1RM LIRT as their intervention [33]. In addition, all of the included studies utilized a moderate training frequency of two or three sessions per week.
Methodological quality and risk of bias
The assessment of methodological quality in the included studies revealed scores ranging from 5 to 7, signifying a classification of ‘good’ methodological quality. It is worth noting that two assessment elements, “blind subjects” and “blind therapists,” were not scored in any of the included studies. This is because, during the intervention, both subjects and therapists were explicitly informed of the allocation of the training and control groups; therefore, blinding could not be implemented. A summary of the methodological quality of the included studies is provided in Table 3.
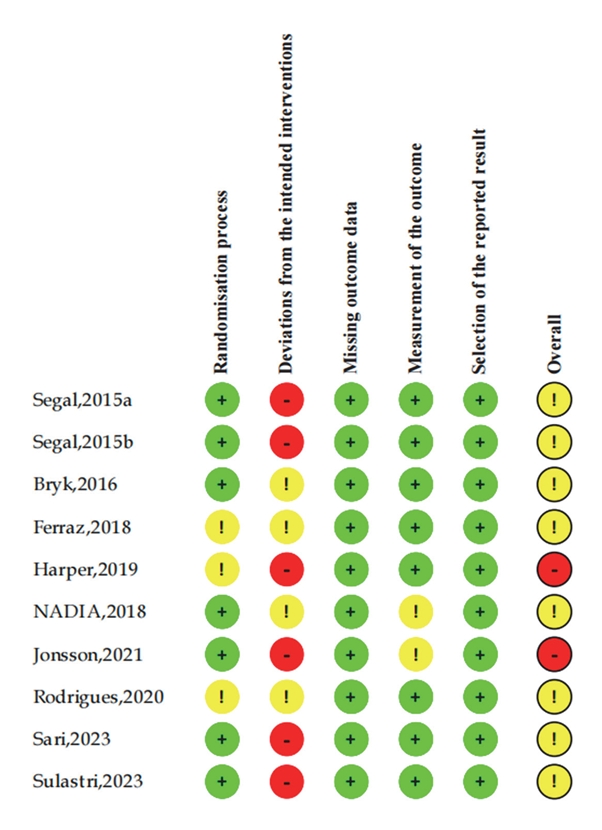
The risk of bias in the included studies was assessed using RoB2.0. The findings revealed that most studies were classified as having either a medium or high risk of bias. Notably, the “Randomization process” and “Deviations from the intended interventions” domains were the primary sources of bias. A summary of the risk of bias in the included studies, along with the corresponding percentages, is presented in Figures 2.1 and 2.2.
Primary outcomes
Pain outcomes
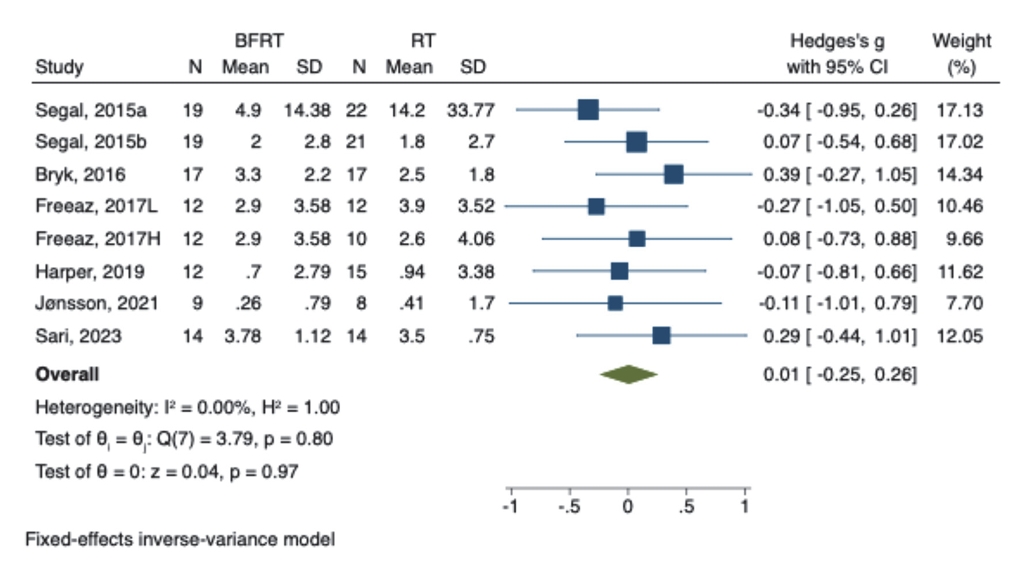
Meta-analysis of pain outcomes showed no heterogeneity between the included studies when comparing BFR + LIRT with RT (I² = 0.00%, Q = 3.79, p = 0.80). The combined effect size showed a lack of statistical significance in the results (SMD = 0.01, 95% CI: -0.25 to 0.26). Figure 3 shows a forest plot of the meta-analysis of the pain outcomes.
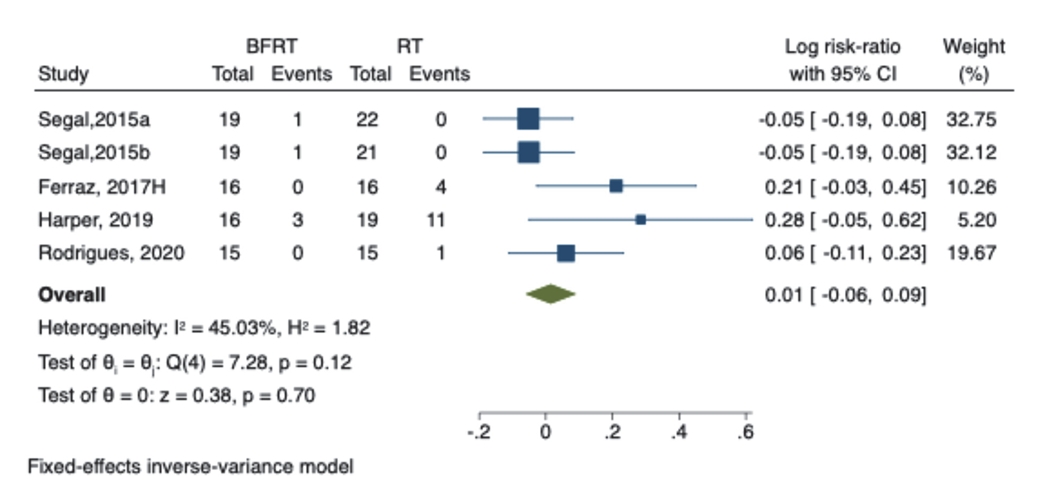
Adverse event outcomes
Of the included studies, five reported adverse events that occurred in subjects as a result of the intervention, mainly in the form of pain and intolerance to the intervention, and Table 2 details the number and causes of adverse events. The meta-analysis comparing the risk ratios of adverse events for BFR + LIRT and RT showed low heterogeneity across studies (I² = 45.03%, Q = 7.28, P = 0.12). Pooling showed that there was no difference in the risk of adverse events between the two training regimens (log RR = 0.01, 95% CI: -0.06 to 0.09). Figure 4 shows a forest plot of the meta-analysis of the adverse event outcomes.
Secondary Outcomes
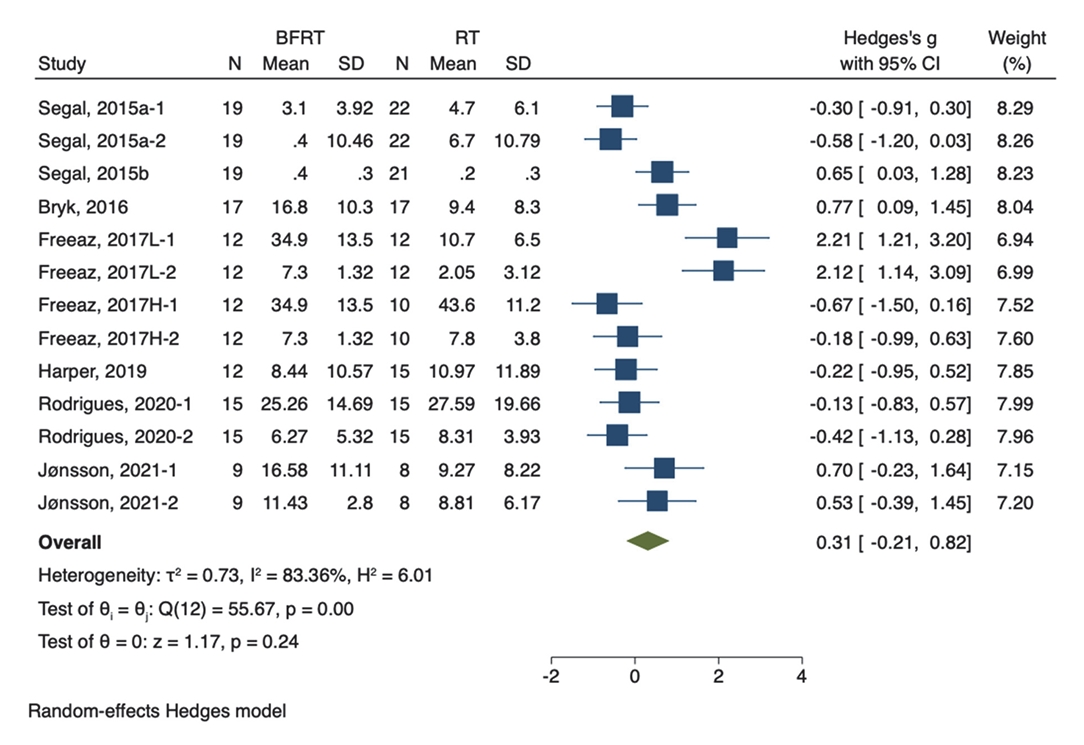
Muscle strength outcomes
The meta-analysis of muscle strength results showed a high degree of heterogeneity among the included studies in the comparison between BFR + LIRT and RT (I² = 83.36%, Q = 55.67, p < 0.01). The results showed that there was no difference between the two training regimens in terms of improving muscle strength (SMD = 0.31, 95% CI: -0.21 to 0.82). Figure 5 shows a forest plot of the meta-analysis of muscle strength outcomes.
Self-reported function
The meta-analysis of self-reported functional outcomes regarding BFR + LIRT versus RT revealed no heterogeneity among the studies (I² = 0.00%, Q = 3.45, p = 0.49). The meta-analysis showed that there was no difference between the two training regimens in improving self-reported function (SMD = -0.06, 95% CI: -0.39 to 0.27, Z = -0.37). Figure 6 shows a forest plot of the meta-analysis of the self-reported functional outcomes.
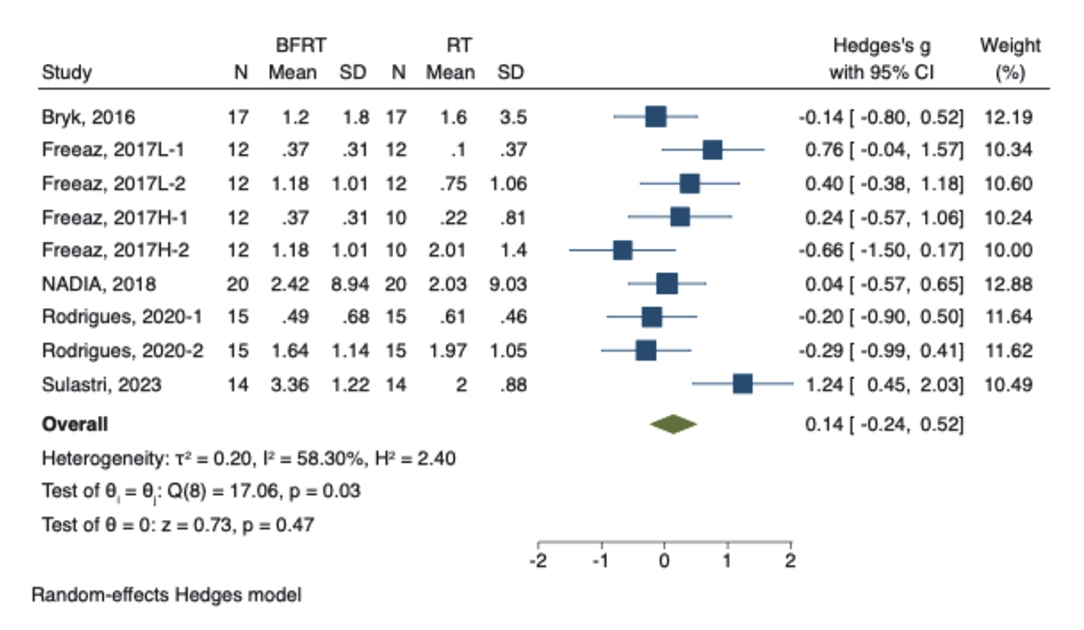
Physical function
A meta-analysis of physical function outcomes showed a high degree of heterogeneity among the included studies when comparing BFR + LIRT with RT (I² = 58.30%, Q = 17.6, p = 0.03). The meta-analysis showed that there was no difference between the two training regimens in improving physical function (SMD = 0.14, 95% CI: -0.24 to 0.52, Z = 0.73). Figure 7 shows a forest plot of the meta-analysis of the physical functional outcomes.
Sensitivity analyses
LOOCV sensitivity analyses were performed to assess the highly heterogeneous muscle strength and physical function outcomes. The results of the sensitivity analyses showed that the ES remained relatively stable despite heterogeneity, highlighting the robustness and reliability of the muscle strength and physical function outcomes. Figures 8 and 9 show the results of the sensitivity analyses of muscle strength and physical function.
Subject analyses
To further explore the sources of heterogeneity and explain the differences in intervention effects between these subgroups more accurately, subgroup analyses were conducted for training intensity, disease type, sex, and measurement method. The results of the subgroup analyses showed significantly less between-study heterogeneity in the subgroup of muscle strength for BFR + LIRT vs. LIRT (83.36% vs. 40.12%, respectively). In addition, a significant improvement in physical function was found in the BFR + LIRT group compared with the LIRT group. In contrast, BFR + LIRT was associated with a lower risk of adverse events than HIRT. In addition, subgroup analyses of the other outcomes were consistent with the results of the pooled analyses. Table 4 shows the results of the subgroup analyses.
DISCUSSION
This systematic review and meta-analysis aimed to provide a larger number of studies and additional outcome metrics to further explore the impact of BFR + LIRT in the clinical management of patients with OA and RA. The results of the study showed that BFR + LIRT had similar effects as RT in terms of increasing muscle strength and improving function, which is consistent with the results of previous studies. However, there was no significant difference between the two training modalities in terms of knee pain reduction or adverse knee events. The results of the subgroup analysis showed that the use of BFR + LIRT was safer than HIRT. In addition, the results of the subgroup analysis showed that BFR + LIRT was superior to LIRT in terms of improving physical function.
Patients with OA and RA often experience pain as a major symptom. This pain not only diminishes the quality of life but can also lead to muscle atrophy and functional impairment [40]. Baseline pain levels are strongly correlated with prognostic outcomes, and improving pain is a major concern for these patients [3,49]. The results of the meta-analysis showed that BFR + LIRT did not demonstrate a significant advantage over RT alone, which was further supported by the results of the subgroup analysis. Of concern, the study by Harper et al. [34] found that baseline knee pain was significantly lower in patients who received BFR + LIRT than in those who received RT, which implies that the baseline assessment introduced an internal bias that may affect the accuracy and reliability of the results of this meta-analysis. Therefore, future studies should explore the applicability and efficacy of BFR + LIRT in joint pain management to fully assess its potential role. Joint pain is also a common adverse event, and age is one of the main factors triggering OA and RA [3,4]. Age is often accompanied by complications such as decreased bone density and muscle mass, leading to questions regarding the safety of training programs that are difficult to control in the management of OA and RA rehabilitation [50,51]. In all of the studies included in the meta-analysis, training-related or potentially training-related adverse events included those related to joint pain and the inability to tolerate the training program. Pooled analyses showed no significant difference in the risk of adverse events between BFR + LIRT and RT. However, in the subgroup analysis of different loads, BFR + LIRT was associated with a lower risk of adverse events than HIRT, suggesting that BFR + LIRT is safer for patients with OA and RA. In addition, Harper et al. [34] reported that the number of adverse events in the group receiving BFR and the group receiving RT was 3 and 11, respectively. This implies that BFR + LIRT is more acceptable to patients, with a similar result reported by Ferraz et al. [33]. Therefore, BFR + LIRT could be an effective clinical rehabilitation tool for patients with OA and RA who are unable to tolerate high-load training. However, Bryk et al. [32] did not explicitly report the group or severity of adverse events, which may have introduced internal bias and reduced the credibility and generalizability of the meta-analysis results. In addition, the credibility of the results is reduced because of the limited number of studies included. Therefore, future studies should include more high-quality studies and more detailed reporting of results as well as a more comprehensive update of the meta-analysis to improve the credibility of the results.
Increased muscle strength was strongly associated with relief of joint discomfort and improved joint stability in patients with OA and RA and also contributed to improved dysfunction [41,42]. The results of the pooled analysis showed a high degree of heterogeneity (I² = 83.36%), with no advantage of BFR + LIRT over RT in terms of increased muscle strength. A sensitivity analysis verified the robustness of the combined results. Subsequent subgroup analyses showed that the heterogeneity of the effect of LIRT on muscle strength decreased to a low level (I² = 40.12%) compared to that of BFR + LIRT, suggesting that the intervention load was one of the main sources of heterogeneity. Training programs are among the most important factors that influence muscle strength. In fact, several studies have favored the inclusion of leg presses and knee extensions, which are crucial for the rehabilitation of patients with OA and RA [43,44]. In addition to the training program, Harper et al. [34] added calf flexion and leg rolls, whereas Bryk et al. [32] added hip abduction and external rotation. These additional exercises may have stimulated the muscles to produce more adaptations, leading to increased heterogeneity between the studies. The key mechanisms of BFR include hypoxia and restricted blood flow, which may increase muscle strength and muscle mass [45,46]. The tourniquet pressure is a pivotal factor influencing the extent of hypoxia and restricted blood flow [47]. The tourniquet pressures used in the included studies were inconsistent; one study used AOP, two studies used 70% LOP, three studies used fixed tourniquet pressures, and four studies used pneumatic cuff pressure. Additionally, cuff specifications can affect BFR outcomes [48]. Among the included studies, four reported cuff widths less than 7 cm, four reported cuff widths greater than 17 cm, and two did not explicitly report cuff widths. Given that these parameters may play a key role in interstudy heterogeneity, future studies should delve deeper into the effects of these factors and determine the optimal training program and BFR parameters. This could lead to a better understanding of the differential effects of these parameters on intervention outcomes, and thus provide more precise recommendations for clinical practice.
Functional impairment can significantly affect the physical activity levels and quality of life of patients with OA and RA, underscoring the critical importance of improving functional impairment in these populations. Considering that these patients often experience joint damage, a moderate training load is crucial. Although high-intensity training has notable effects on functional improvement, it also poses potential risks. The meta-analysis revealed no significant differences in self-reported functional improvement between the LIRT + BFR and RT groups, a finding corroborated in terms of physical function. However, the subgroup analysis revealed a significant improvement with BFR + LIRT compared to RT. Compared to HIRT, the improvement effect of BFR + LIRT showed no significant difference, further validating its potential in patients with OA and RA. Considering the relatively safer profile of BFR + LIRT compared with HIRT, this suggests that BFR + LIRT is a viable disease management option.
The PEDro scale was used to objectively assess the quality of the included studies. The results of the assessment showed that most of the studies scored as “good” quality, confirming their reliability. However, most studies scored low on the items “blind subjects” and “blind therapists.” This resulted from the fact that both the intervention and control groups received actual training, and both participants and therapists were aware of the type of training they received and therefore could not be blinded. It is worth noting that the Harper et al. study may have exposed the absence of “blind subjects.” In that study, the BFR + LIRT group had a perceived exertion score of 7.3 ± 0.5, whereas the RT group had a perceived exertion score of 8.1 ± 0.5, suggesting that participants in the RT group exerted more effort during training compared to the BFR + LIRT group, which may have resulted in more favorable outcomes, which in turn may have biased participants or therapists toward the intervention they received [34]. On the other hand, the RoB 2.0 risk of bias assessment showed that three studies were categorized as some concern risk in the area of “randomization process” because they did not report the allocation concealment method [33,34,37]. In the area of “outcome measures,” two studies were categorized as some concern risk because they did not report blinded assessors [35,36]. The results of these assessments emphasize the need for careful interpretation when considering aggregation to accurately assess the reliability of studies.
This study has some limitations. Few studies have previously implemented BFR + LIRT in patients with OA and RA, which may have affected the stability of the results. Rigorous blinding could not be implemented because the participants and therapists were explicitly informed about the training program, resulting in some bias. The participants included in the study were predominantly female, which may have limited the exploration of the effectiveness of training participation among male participants, as well as the generalizability of the results. There were also constraints on the characteristics of the interventions, including inconsistencies in elements such as the training program, BFR parameters, and training duration, which may have increased the heterogeneity between studies. Furthermore, there were inconsistencies in the measurement methods applied in the included studies, which may also have led to heterogeneity between the measurements. Despite these limitations, this study contributes to a deeper understanding of the effects of BFR + LIRT on pain reduction in patients with OA and RA. Future studies should aim to overcome these limitations in order to provide more comprehensive analyses and enhance our understanding of these issues.
This systematic review and meta-analysis further supports the potential of BFR + LIRT in the disease management of patients with OA and RA. According to this analysis, BFR + LIRT had a lower risk of adverse events than HIRT and may be a safer training modality. BFR + LIRT offers greater advantages in improving physical function than LIRT and was able to provide similar benefits to HIRT without increasing the training load. These findings suggest that BFR + LIRT is a safe and effective strategy for treating patients with OA and RA. However, owing to the limited number of studies covered in this analysis, additional higher-quality studies are needed to strengthen this conclusion.
Acknowledgements
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2022R1F1A1063548).
This study was supported by the KU Research Professor Program of the Konkuk University.