Effect of pilates training on pain and disability in patients with chronic low back pain: a systematic review and meta-analysis based on randomized controlled trials
Article information
Abstract
[Purpose]
This systematic review and meta-analysis study evaluated the effects of Pilates on pain and disability in patients with chronic low back pain.
[Methods]
Six electronic databases were searched between January 2012 and December 2022. From these databases, only randomized controlled trials were selected. The criteria for assessing methodological quality using the PEDro scale were selected. The risk of bias was assessed using the Cochrane Risk of Bias Tool RoB 2.0. Additionally, the primary outcomes were pain and disability in this analysis.
[Results]
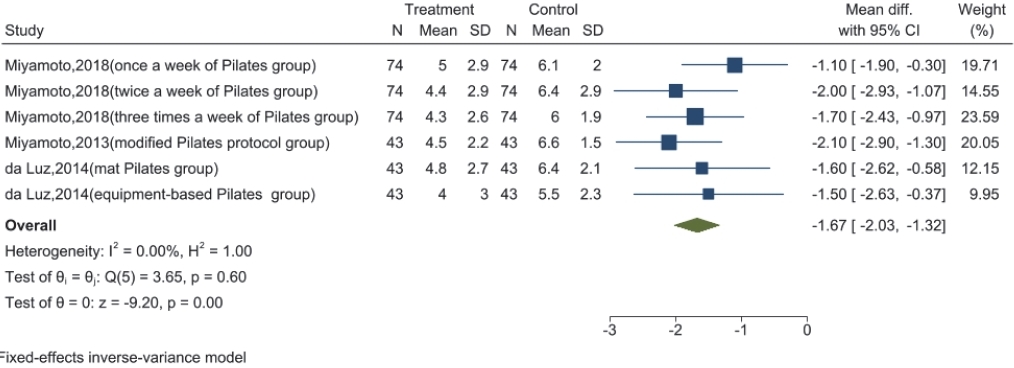
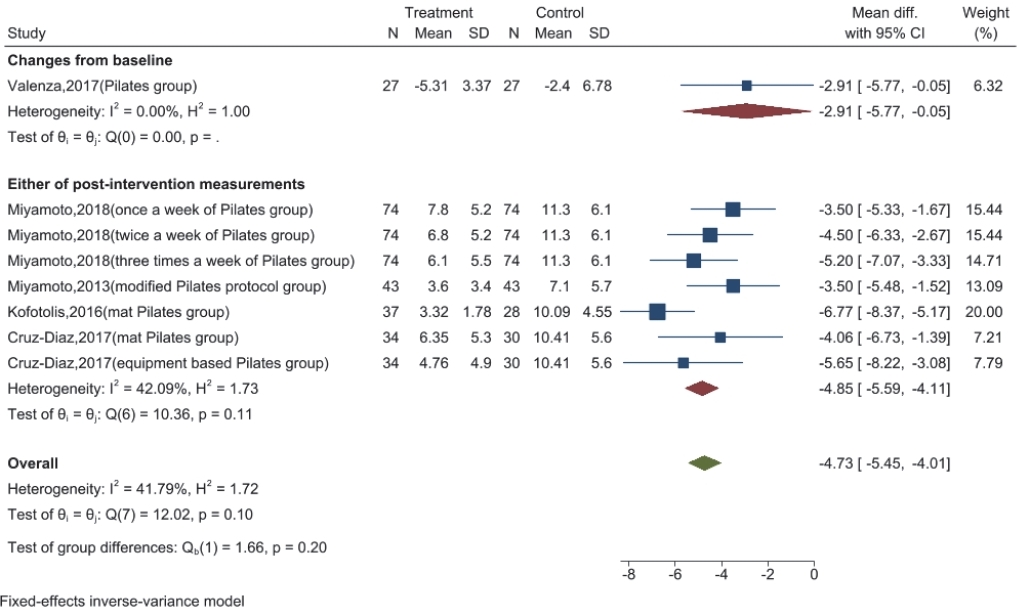
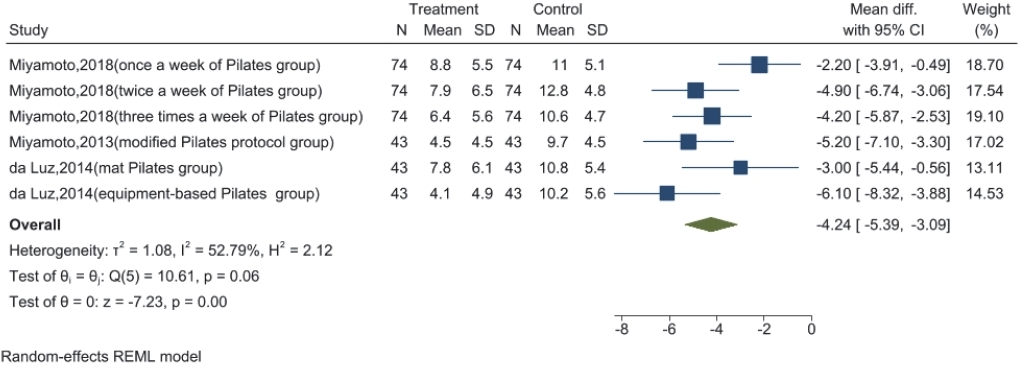
The corresponding results confirmed that Pilates training led to a significant improvement in pain (Visual Analog Scale: weighted mean difference = -29.38, 95% confidence interval, -33.24 to -25.52, I2 value = 56.70%; Pain Numerical Rating Scale: weighted mean difference = -2.12, 95% confidence interval, -2.54 to -1.69, I² value = 0.00%) and disability (Roland– Morris Disability Index: weighted mean difference = -4.73, 95% confidence interval, -5.45 to -4.01, I² value = 41.79%). Six months after completion of Pilates training, the improvement in pain (Pain Numerical Rating Scale: weighted mean difference = -1.67, 95% confidence interval, -2.03 to -1.32, I2 value = 0.00%) and disability (Roland–Morris Disability Index: weighted mean difference = -4.24, 95% confidence interval, -5.39 to -3.09, I2 value = 52.79%) was maintained.
[Conclusion]
Pilates training may be an effective strategy to improve pain and disability in patients with chronic low back pain.
INTRODUCTION
Low back pain (LBP) is one of the most common musculoskeletal disorders worldwide, with a lifetime prevalence of approximately 40% [1]. LBP is primarily characterized by increased pain and functional impairment and is, therefore, one of the top 10 causes of disability across all age groups [2,3]. The number of people experiencing LBP worldwide was approximately 377.5 million in 1990; however, by 2017, the number of people with LBP had increased to approximately 577 million worldwide (prevalence: 7.5%), with an ageing population being one of the primary reasons for this significant increase [3,4]. Moreover, a systematic review of the prevalence of LBP in the elderly reported a 21–75% prevalence of LBP among those over 60 years of age [5]. Additionally, owing to the worldwide prevalence of COVID-19, people are less physically active, leading to a significant increase in the incidence and intensity of LBP [6]. Currently, LBP causes significant economic losses worldwide every year, especially in low- and middle-income countries, where LBP is more likely to lead to disability. The consequential cost of medical care and loss of productivity due to LBP is extensive and poses a serious burden on society and the economy [2,7,8].
Approximately 5.0–10.0% of patients with LBP may progress to chronic low back pain (CLBP) [9]. Many patients with CLBP are identified as having nonspecific chronic low back pain (NSCLBP), characterized by an inability to identify the cause of the pain [13,14]. In fact, CLBP may be considered more difficult to treat than acute LBP [10]. CLBP typically lasts for more than three months and often interferes with daily life and work owing to persistent pain and functional limitations; therefore, patients with CLBP require long-term treatment with ongoing management [2,55]. Exercise-based training has been established as an effective treatment for CLBP [11,18]. Further, Pilates training is gaining acceptance as one of the most popular exercise programs in this context [19]. Pilates training is a comprehensive exercise movement technique that has been shown, in several previous randomized controlled trials (RCTs), to significantly improve pain, disability, and quality of life in patients with CLBP [33,35,42,43,45]. Pilates training is characterized by significant effects in activating the core muscle groups, enhancing the stability of several body regions, and improving the mobility of the lumbar joints [57,58]. The core muscles of patients with CLBP, such as the internal oblique, transverse abdominis, rectus abdominis, multifidus, and iliopsoas muscles, are weakened [59]. As these muscles weaken, lumbar stability and lumbar spine mobility diminish. Pilates training reactivates these muscles, enhancing the strength and stability of the lumbar region. In addition, through stretch-based posture and breath control, the range of motion of the lumbar spine can be improved, resulting in improved pain and dysfunction in CLBP patients [60]. Various Pilates training modalities exist, among which mat Pilates training is widely used in the clinical management of patients with musculoskeletal disorders [61]. Mat Pilates includes various positions, such as standing based positions, or can be implemented with additional apparatus. Mat Pilates training is useful for activating core muscles to enhance local stability. Bergson et al. analyzed the implementation of Pilates core stabilization exercises in quadruped position; specifically, they observed a significantly increased activation of the lumbar multifidus, gluteus maximus, rectus abdominis, and internal and external obliques, which ultimately resulted in maintenance of stability in the lumbopelvic region of the participants [62]. Additionally, Kyeongjin et al. indicated that Pilates stabilization exercises were effective in activating the internal oblique, rectus abdominis, multifidus, and iliocostalis lumborum, resulting in increased pelvic and trunk stability [63]. Further, Batibay et al. conducted a mat Pilates training program and a home training program for female CLBP patients and found that core stability and muscle thickness of the lumbar multifidus, transverse abdominal, external oblique, and internal oblique rectus muscles were significantly higher in the Pilates group [37]. Overall, mat Pilates is effective in activating core muscles and improving low back and pelvic stability, even in CLBP patients. On the other hand, apparatus Pilates training is becoming more popular [35,36]. Apparatus Pilates reduces the period in which individuals are in a standing position and, therefore, reduces the load of holding up the body weight. Simultaneously, by increasing the resistance of the apparatus during the training load of the exercise can be increased, which can confer an additional activating effect on the muscles. Therefore, apparatus Pilates can provide additional improvements in strength training for the treatment of patients with CLBP. da Luz et al. conducted a trial that analyzed mat and apparatus Pilates in patients with NSCLBP and found significant improvements in pain, disability, and kinesiophobia in both groups by the end of the session, with interim follow-up results showing significant improvements in the apparatus Pilates group [35]. Cruz-Diaz et al. performed mat and apparatus Pilates training in patients with CLBP. Both groups achieved significant improvements in transversus abdominis activation rates; however, a long-term follow-up after training indicated that only the patients in the apparatus Pilates group maintained the improvement in the transversus abdominis activation rate [36]. These results suggest that apparatus Pilates may be superior to mat Pilates for the treatment of CLBP. In addition, water Pilates is commonly used in clinical trials. Similar to water aerobics, Pilates training in water reduces the potential for injury and the impact of physical loading. In addition, owing to the resistance of water, the external exercise load also increases [64,69]. Yalfani et al. indicated that there were similar pain and functional improvements in NSCLBP patients that participated in mat or water Pilates [39]. This suggests that water Pilates may be an effective training modality for NSCLBP patients. These different Pilates training modalities may lead to different results from those of previous studies. Additionally, Pilates training appears to be superior to other exercise therapies for the treatment of CLBP. Specifically, a network meta-analysis indicated that Pilates training was more effective in improving pain and function than other effective treatments and exercise types [15]. Although some studies have reported more favorable results for Pilates training in the treatment of patients with CLBP, others continue to suggest that the effectiveness of Pilates training for CLBP remains controversial. Several systematic reviews have indicated that Pilates training did not improve pain or function, or only improved pain with no significant effect on function [16,17,19]. The discrepancies in these results may be attributed to the fact that these studies were published relatively early; therefore, these systematic reviews analyzed fewer studies, which may have affected the accuracy of the results. There are many studies on the incorporation of mat Pilates in previous studies; however, few studies implement the analysis of water or apparatus Pilates. This may have led to discrepancies between the results of the present study and those of previous systematic evaluations and meta-analyses. In addition, previous studies did not explain the short- and medium-term clinical significance of Pilates training for improving pain and disability in patients with CLBP. This may create confusion for medical professionals regarding the choice of Pilates training for treatment.
Therefore, the purpose of this study was to examine the short- and medium-term effects of Pilates training on pain and disability in patients with CLBP and to explore its corresponding clinical implications.
METHODS
Study design
This systematic review and meta-analysis were conducted according to the recommendations of the Cochrane Handbook, and was designed according to the PRISMA guidelines, the preferred reporting item for systematic review and meta-analyses, and a standard process design [20,21].
Search strategy
Six electronic databases, MEDLINE (via PubMed), Embase (via Scopus), Web of Science, Proquest Central, Physiotherapy Evidence Database (PEDro), and the Cochrane Central Register of Controlled Trials were selected to conduct a systematic search of Pilates training in patients with CLBP. To develop search terms, “Pilates” and “CLBP” were selected through the National Center for Biotechnology Information to search in medical subject headings (MeSH), free words and matching synonyms, and for the use of Boolean operators “OR” and “AND” to link the search terms. It is important to note that the search terms for this study were limited to the titles and abstracts. In addition, we evaluated all studies published over the last 10 years. Studies that were not reported in English were included to ensure that relevant studies were not omitted. The search process concluded on November 20, 2022, and the results were saved in EndNote X9 (Clarivate, London, UK).
Inclusion/exclusion criteria
Inclusion criteria
The inclusion criteria of this meta-analysis were as follows: (1) Population: studies in which the mean age of participants was ≥18 years and the duration of CLBP was >12 weeks; (2) Intervention: studies in which participants were assigned to at least one Pilates group of any kind; (3) Outcome: studies in which the outcome measure was a pain or disability index measurement tool and scale; and (4) Study design: studies of complete RCTs from any source (including gray literature).
Exclusion criteria
Studies were excluded if: (1) Participants included those under 18 years of age or special populations (e.g., pregnant women); (2) Studies in which the participants underwent <4 weeks of training; (3) Studies that reported results that did not allow calculation of effect sizes for the data; and (4) Studies rated as poor by the PEDro scale for methodological quality.
Data extraction
Eligible study data were extracted after full-text inspection. The extracted data included the author’s names, year of publication, details regarding participants (sample size, age, and type of disease), frequency and length of the Pilates training, and measurement outcomes (pain and disability). Extracted data were stored in a Microsoft Excel table.
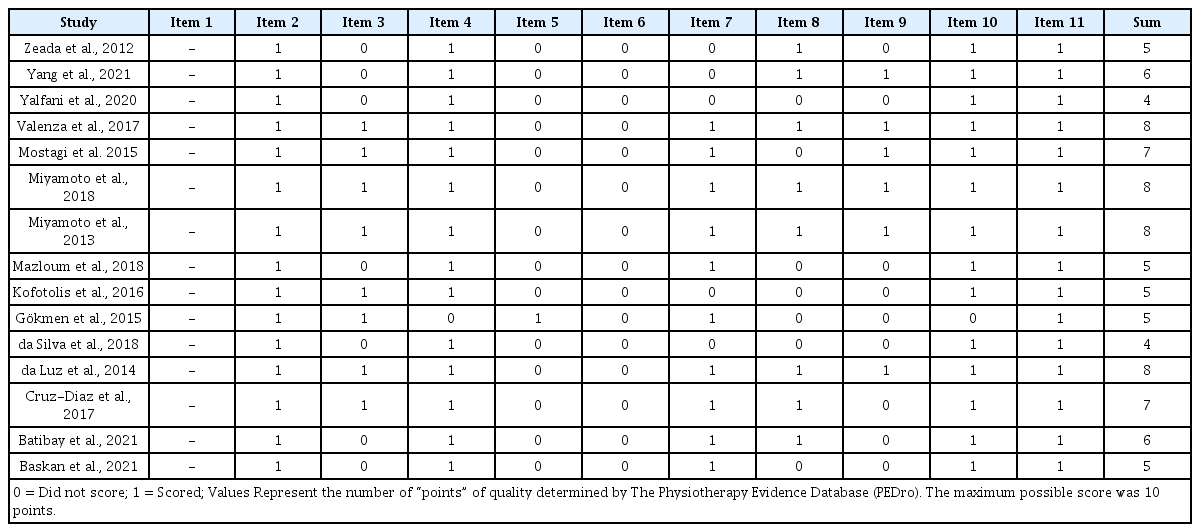
Methodological quality assessment
The methodological quality of the studies was assessed using the PEDro scale. The PEDro scale includes 11 items with a total score of 10; specifically, these 11 items consider external validity (item 1), internal validity (items 2–9), and statistical reporting (items 10–11), with item 1 not being included in the calculation of the total score. If the criteria were met, the score was assigned to the corresponding category in the present study. A final total score of 0–3 was considered “poor,” 4–5 was considered “fair,” 6–8 was considered “good,” and 9–10 was considered “excellent” [22].
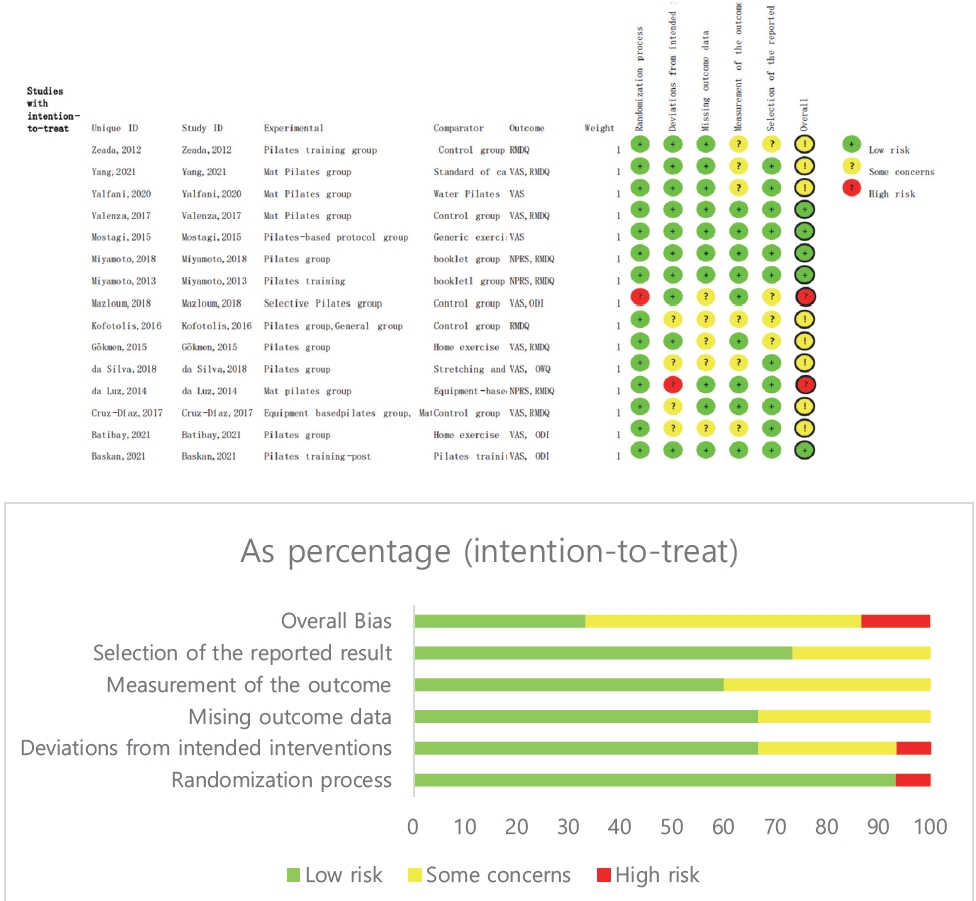
Assessing the risk of bias
The risk of bias in RCT studies was assessed using the Risk of Bias in RCTs tool 2.0 (RoB 2.0) from the Cochrane Collaboration. RoB 2.0 is considered to be a reliable tool for detecting the risk of bias in RCTs. The randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of reported results were examined. These questions were rated as yes (Y), probably yes (PY), no information (NI), probably no (PN), or no (N)23. Finally, these questions are summarized and were classified as low, medium, or high risk of bias [23].
Statistical analysis
The outcomes of both pain and disability were expressed as continuous variables. For between-group comparisons, data on the mean difference and corresponding standard deviation of change from the baseline were selected for extraction as a priority for inclusion in the study [21]. If this was not possible, the mean and standard deviation of the post-intervention measures were extracted and combined by subgroup analysis; additionally, if the direction of change from the baseline differed from that of the instrument or scale, the data from the mean and standard deviation were multiplied by minus one to correct the direction [21]. For within-group comparisons, the pre-intervention baseline mean and standard deviation and post-intervention final mean and standard deviation data were selected for extraction. It is important to note that studies evaluating short-term effects were selected for outcome data closest to the end of the trial intervention; further, studies evaluating the intermediate effects of Pilates were preferred over those that assessed outcome data six months after the end of the trial intervention [24,25]. Additionally, if studies did not report the means and standard deviations, priority was given to contacting the authors to obtain raw data. If no response was received from the authors, these differences were calculated using the methods recommended in the Cochrane handbook. When the data were expressed as the median and interquartile range, utilized the following formula for the conversion of the mean [21,26]:
where q1, m, and q3 are the first quartile, median, and third quartile, respectively. Further, the standard deviation was determined using the interquartile range and the following formula [26]:
In this study, effect sizes (ES), I2 values, and 95% confidence intervals were calculated using STATA (version 17, Stata Corp.). The weighted mean difference was used to calculate effect size when using the same instrument or scale. The I² value was selected to determine between-study heterogeneity: 0–40%: likely insignificant; 30–60%: likely represents moderate heterogeneity; 50–90%: likely represents significant heterogeneity; 75–100%: significant heterogeneity21. The combination of effect sizes and the 95% confidence interval were chosen to determine statistical significance; if the 95% confidence interval did not intersect the null line and both the effect size and 95% confidence interval fell to the left of the null line, the results were considered favorable for the experimental group [27-29]. It is important to note that in terms of model selection, inverse variance fixed-effects models should be used for between-group comparisons [21]. For within-group comparisons, a fixed-effects model was chosen if the I2 value was < 50%. Otherwise, a random effects model was used [30]. In addition, if the heterogeneity of the results were high, the heterogeneity of each study and the stability of the analysis were tested using sensitivity analysis. This was performed by removing each study individually to detect whether there was a significant change in heterogeneity to determine the overall robustness of the results [31].
RESULTS
Search results
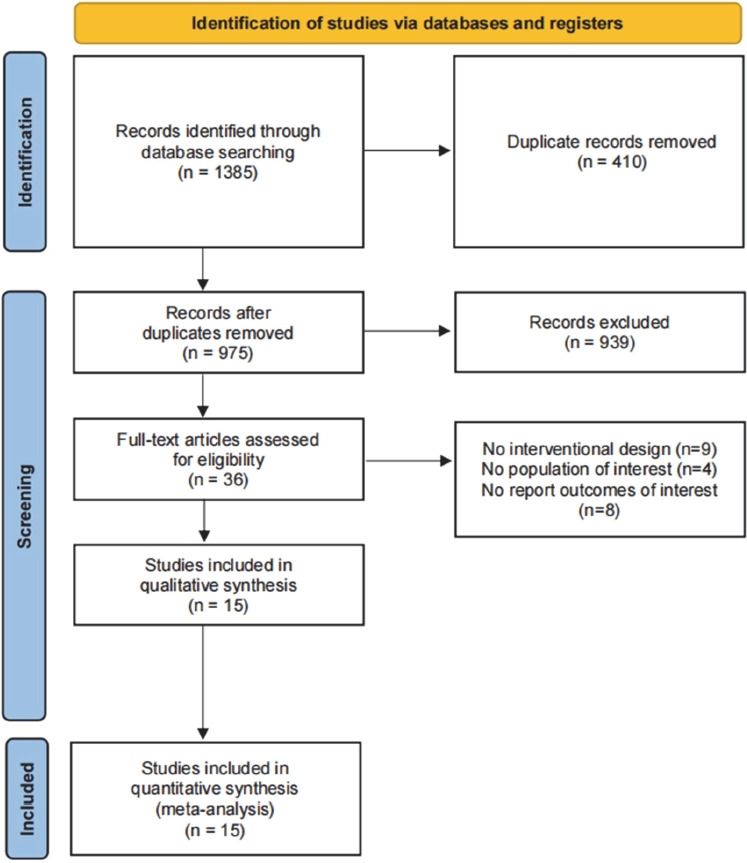
Following the electronic database search for relevant studies, a total of 1385 study titles and abstracts were obtained. Then, after examining duplicate studies, 410 duplicate studies were excluded, leaving 975 non-duplicate studies. Next, after checking the titles and abstracts of the remaining studies, 939 were excluded, which left a remaining 36 studies. After full-text examination of the remaining 36 studies, 8 studies were excluded because the reported outcomes did not meet the inclusion criteria, 4 studies were excluded because the subjects did not meet the inclusion criteria, and 9 studies were excluded because the intervention design did not meet the inclusion criteria; this left a total of 15 studies. Finally, a systematic review and meta-analysis could be conducted utilizing the remaining 15 studies [32-46]. The flow of this selection process is summarized in Figure 1.
Characteristics of the studies
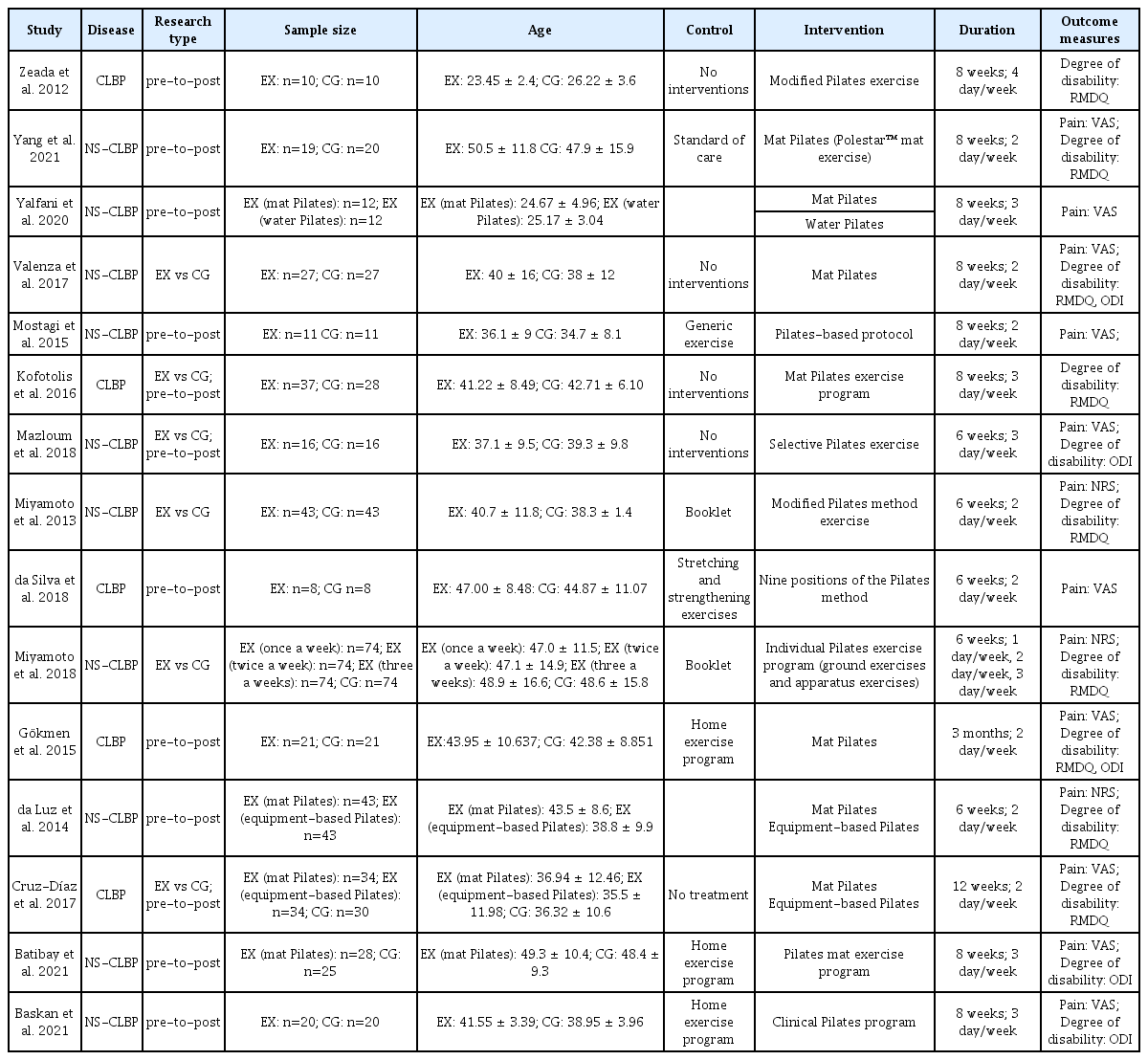
All 15 included studies were RCTs. Of these, one study was a “gray literature” study (6.67%) [46]. The remaining 14 studies were published in journals (93.33%) [32-45]. All the included studies were published between 2012 and 2022.
Participants
Of the 15 included studies, there were 973 participants, of which 640 (65.78%) were in the experimental group and 333 (34.22%) were in the control group. The number of participants in each of the included studies ranged from 8–74. The mean age of all subjects in these studies was 23–50 years. Table 1 provides more detailed information on participant characteristics.
Intervention
In 5 of the 15 included studies, subjects either performed non-Pilates training, did not participate in any activity, did not receive a specific exercise prescription, or only received pamphlet. The experimental group underwent four forms of Pilates training across these studies: mat, water, and apparatus Pilates. The average frequency of the Pilates training sessions ranged from one to four times a week. The duration of the trials ranged from 6 to 12 weeks (1.5–3 months). Table 1 provides detailed information on the intervention characteristics.
Outcomes
Among the 15 included studies, the primary outcome indicators were pain and disability. The methods chosen to report pain were the Visual Analog Scale (VAS) and the Pain Numerical Rating Scale (NRS), which are considered reliable tools for assessing LBP [47]. Alternatively, the methods used to report disability outcomes were the Roland– Morris Disability Questionnaire (RMDQ) (Cronbach α = 0.92) and the Oswestry Disability Index (ODI) (Cronbach α = 0.90), which were considered reliable for the assessment of disability in patients with LBP [48,49].
Risk of bias
The risk of bias of these RCTs was assessed using RoB 2.0. The corresponding results demonstrated that two RCTs (13.33%) had a high risk of bias [35,44], eight RCTs (53.34%) had a medium risk of bias [32-34,36,37,39,45,46], and five RCTs (33.33%) had a low risk of bias [38,40-43]. Figure 2 provides detailed information on this risk of bias assessment.
Pain outcomes
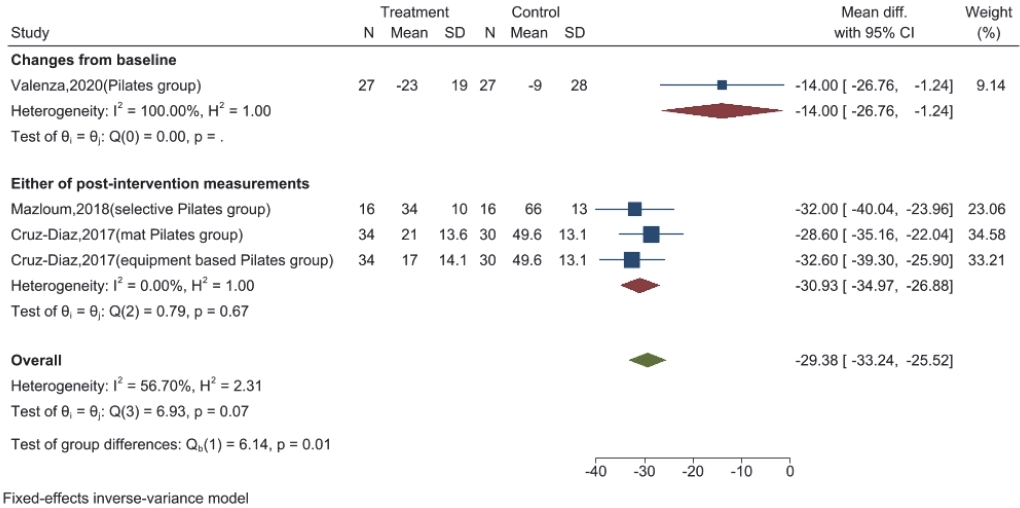
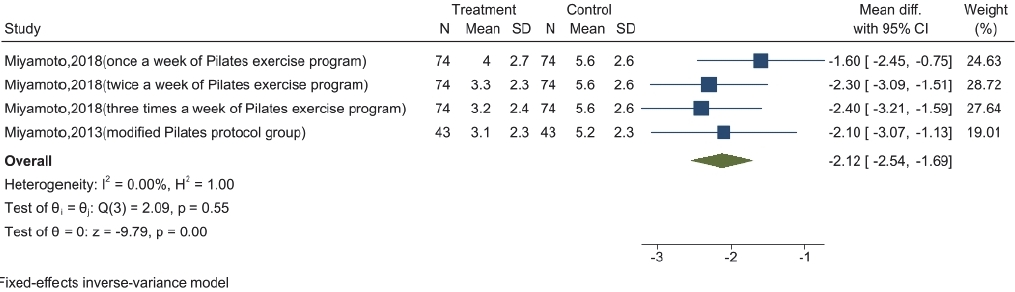
Twelve studies reported on pain outcomes [33,34,36-44,46]. Of these, three studies reported VAS outcomes with Pilates training compared to minimal interventions [36,40,44]. Alternatively, two studies reported NRS outcomes [42,43]. The VAS confidence interval was 0–100 mm and the minimum clinically significant difference was 17–18 units [50]. The NRS confidence interval was 0–10 points and the minimum clinically significant difference was 2 units [51]. VAS outcomes were significantly lower in the Pilates group than in the minimal intervention group (weighted mean difference = -29.38, 95% confidence interval, -33.24 to -25.52, I² value = 56.70%) (Figure 3). Similarly, there was a significant reduction in the NRS in the Pilates group compared to that in the control group (weighted mean difference = -2.12, 95% confidence interval, -2.54 to -1.69, I² value = 0.00%) (Figure 4). Overall, these changes were considered clinically significant.
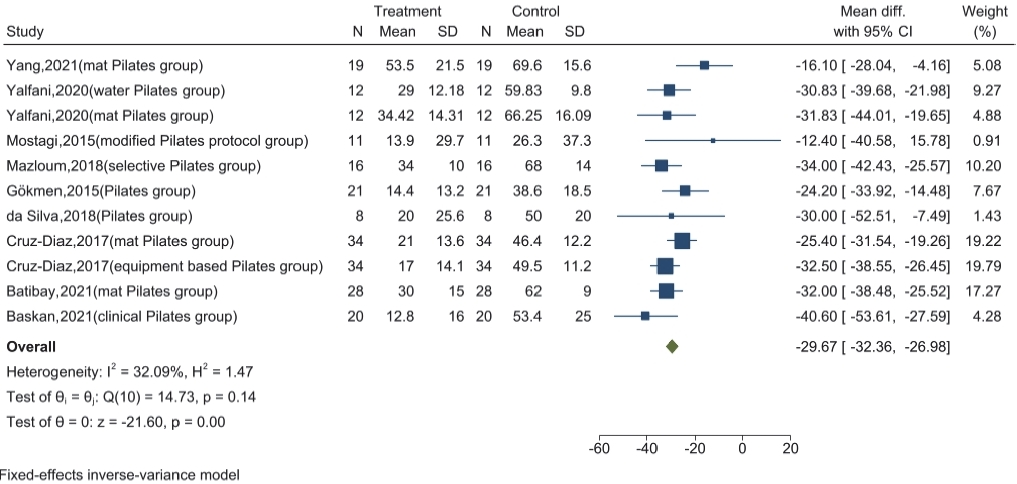
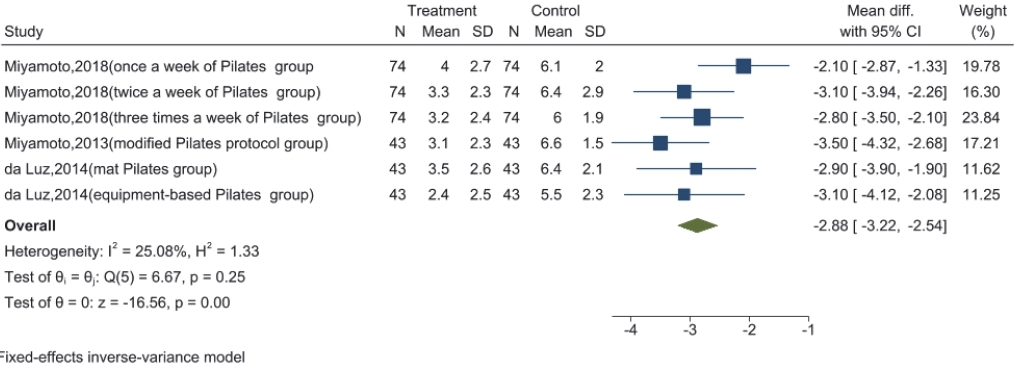
Nine studies reported on VAS outcomes after Pilates training; corresponding statistically significant and clinically meaningful short-term improvements were observed after Pilates training (weighted mean difference = -29.67, 95% confidence interval, -32.36 to -26.98, I² value = 32.09%) (Figure 5) [33,34,36-39,41,44,46]. Further, three studies reported on NRS pain outcomes at the end of Pilates training and 6 months after training [35,42,43]. Overall, a significant improvement in short-term pain relief after Pilates training was found (weighted mean difference = -2.88, 95% confidence interval, -3.32 to -2.54, I² value = 25.08%) (Figure 6). Although pain relief was also evident in the mid-term after Pilates training, this change was not clinically significant (weighted mean difference = -1.67, 95% confidence interval, -2.03 to -1.32, I² value = 0.00%) (Figure 7).
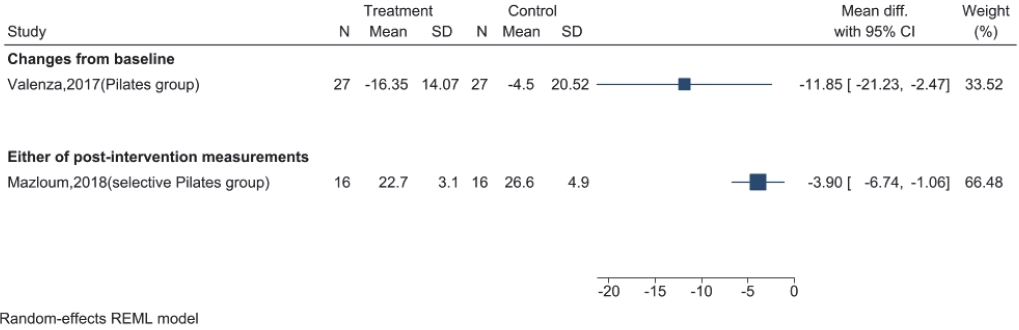
Disability outcomes
Six of the fifteen studies reported disability outcomes for Pilates training compared with minimal interventions [36,40,42-45]. The ODI range was between 0–50 points, with a clinically significant difference of 9.5 units. Additionally, the RMDQ range was 0–24 points, with a clinically significant difference of 3 units [52,53]. The ODI results for the Pilates training were compared to the minimal intervention group due to the small number of studies; therefore, the use of “post-intervention measures” and “change from baseline” were used to express these results. Consequently, to avoid misleading results, we omitted the pooled effect size (Figure 8). Nonetheless, the Pilates training group demonstrated a statistically significant reduction and clinically meaningful improvement in RMDQ outcomes compared to that in the minimal intervention group (weighted mean difference = -4.73, 95% confidence interval, -5.45 to -4.01, I² value = 41.79%) (Figure 9).
Eight studies reported disability outcomes for the RMDQ after Pilates training was concluded [32,33,35,36,42,43,45,46]. Overall, a significant improvement in short-term disability after Pilates training was found (weighted mean difference = -5.46, 95% confidence interval, -6.56 to -4.36, I² value = 72.55%) (Figure 10). Additionally, three studies reported on the RMDQ disability outcomes 6 months after Pilates training; the corresponding significant improvements in disability outcomes midway through Pilates training were considered clinically significant (weighted mean difference = -4.24, 95% confidence interval, -5.39 to -3.09, I² value = 52.79%) (Figure 11) [35,42,43].
Sensitivity analyses
The disability outcome analysis of these studies revealed large heterogeneity. Nonetheless, after removing one study at a time from this analysis, no significant differences in the outcomes were found, indicating robust results.
DISCUSSION
Overall, the results of this systematic review and meta-analysis suggest that Pilates training can improve pain and disability in patients with CLBP. Since these new RCTs have been published in recent years, there have been no relevant studies on the effectiveness and durability of Pilates training for patients with CLBP. Therefore, this systematic review and meta-analysis examined the effects of Pilates training on pain and disability in CLBP patients. The corresponding findings demonstrated that Pilates training resulted in a clinically significant improvement in pain and disability compared to that in minimal interventions. However, within-group comparisons with pre-Pilates training showed a decrease in pain and disability improvement at the end of training in patients that did not implement daily Pilates training interventions after the initial intervention. Nonetheless, although improvements in pain and disability decreased in the mid-term post-training period compared with the short-term period, they remained significantly improved compared with the pre-training period, especially for the corresponding disability index, which remained at an improvement level greater than the minimum value required for clinically significant differences.
The improvement in pain and disability after Pilates training in CLBP patients was compared with minimal intervention. This systematic review and meta-analysis found statistically significant and clinically meaningful improvements in pain and disability after Pilates training in CLBP patients compared with minimal intervention. The corresponding results obtained in the current study differ from those of previous studies. A systematic review and meta-analysis by Pereira et al. [16] indicated that Pilates training did not improve function or pain. Additionally, a systematic review and meta-analysis by Aladro-Gonzalvo et al. [17] indicated that although Pilates provided more than moderate significant pain relief compared to minimal intervention, it did not significantly improve function. Further, Lim et al. [19] indicated that when Pilates-based training was compared with minimal intervention, Pilates training provided a greater improvement in pain but did not support a greater reduction in disability. It should be noted that these studies were published relatively early. Because there have been few recent review studies on the effects of Pilates training in patients with CLBP, new RCTs have not been included in these previous studies. Ultimately, this may have resulted in the previous systematic reviews and meta-analyses being out of date, which may be one reason why the results of this study differ from those of previous studies. In addition, the number of RCTs on the effects of water and apparatus Pilates training has increased in recent years. The implementation of these Pilates training modalities in CLBP patients has achieved significant results similar to those of mat Pilates. In particular, water and apparatus Pilates have been demonstrated to be much more advantageous than mat Pilates in medium-to long-term follow-up after training [35-37]. Therefore, it can be argued that water and apparatus Pilates are more effective than mat Pilates. Since few prior systematic reviews and meta-analyses of water and apparatus Pilates studies were included, this may lead to inconsistencies between the results of the present study and those of previous studies. This may explain the discrepancy between the results of the present study and those of the previous systematic reviews and meta-analyses.
In addition, we analyzed the effect of Pilates training on improving the persistence of pain and disability in CLBP patients. Based on the results of this analysis, there was a statistically and clinically significant improvement in shortterm pain and disability outcomes after Pilates training. As the duration of Pilates training increased, a decrease in pain and disability improvement was observed in the mid-term after Pilates training, with the improvement in pain becoming less than the minimal value required for clinical significance; nonetheless, the effect of Pilates training on disability remained clinically significant. Few RCTs have reported the long-term pain and disability outcomes of Pilates. Nonetheless, Miyamoto et al. indicated a greater reduction in pain and disability improvement outcomes at 12 months after the end of training compared to the short and intermediate post-intervention periods [42,43]. These results suggest that Pilates training is effective in the short and medium term for the treatment of pain and disability in patients with CLBP. However, at the end of the training period, the improvement in pain and disability outcomes decreased over time. Therefore, a longer-term training program is recommended when Pilates training is chosen as a treatment modality for CLBP patients in order to achieve significant improvements in pain and disability.
In within-group analyses of short-term outcomes of disability after training, there was significant statistical heterogeneity in the combined effect size of the RMDQ despite significant improvements in disability. Therefore, sensitivity analyses were performed to determine the robustness of the results of these studies. Nonetheless, no statistically significant improvement was observed after performing sensitivity analyses and excluding any studies, indicating that the results were robust. The reason for this large heterogeneity may be attributed to the differences in methodological quality. Analysis of methodological quality by PEDro revealed thirteen RCTs with scores ≥5 and two RCTs with scores ≤5, which may have led to bias in the results [32-38,39,40,42-46,54]. Second, the characteristics of CLBP patients differed, which was primarily reflected by the different age ranges and sexes. Further, the effects of Pilates training on CLBP patients were observed to differ by age range and sex, potentially leading to bias. Third, the training duration, length of sessions, and frequency of sessions were inconsistent across the RCTs. The average frequency of Pilates training ranged from one to four times per week, session lengths ranged from 40 to 75 min, and trial duration ranged from 6 to 12 weeks. Therefore, CLBP patients who received more Pilates training may have had a greater advantage in disability improvement, which may have resulted in increased heterogeneity of outcomes. Finally, the Pilates training types used varied among these RCTs, with various forms of Pilates training, such as mat, water, and apparatus Pilates. The selection of Pilates training was not identical across the studies, which may have produced heterogeneous results. Therefore, more RCTs are required to confirm these differences.
Pain and disability are the main manifestations of CLBP. Pain outcomes in the lower back are easily assessed using VAS or NRS [47,65]. For the assessment of disability, the ODI determines disability in terms of pain intensity, weight lifting, self-care, ambulation, sitting ability, sexual function, standing ability, social life, sleep quality, and travel ability of the patient [48,66]. Alternatively, the RMDQ assesses disability by focusing on walking, bending, sitting, lying down, dressing, sleeping, self-care, and daily activities. The ODI and RMDQ provide an accurate reflection of the disability experienced by CLBP patients [49,67,68]. In addition to pain and disability, patients with CLBP often have problems with back muscle strength, muscle endurance, joint range of motion, and reduced balance. These problems are typically associated with more severe disabilities and can have an impact on the independence of these patients to perform daily activities [55,56]. RCTs have reported the effects of Pilates training as a comprehensive exercise technique that improves these parameters. Zeada et al. [32] demonstrated that 8 weeks of Pilates training could result in significant improvements in trunk flexion and extension and a significant reduction in urinary mandelic acid secretion, which is associated with strength and explosive adaptations; this suggests that Pilates training in patients with CLBP is effective in improving joint range of motion and increasing muscle strength. Studies conducted by Yang et al. [33] and Kofotolis et al. [45] established that the’ quality of life of CLBP patients improved after 8 weeks of Pilates training, and this improvement was maintained 3 months after training. In a study conducted by Yalfani et al. [39], an 8-week follow-up of the patients established that both water and mat Pilates training had a beneficial effect on improving dynamic and static balance in patients with NSCLBP. Further, Valenza et al. [40] observed significant improvements in lumbar spine mobility and balance in patients with NSCLBP that completed an 8-week Pilates training program. Miyamoto et al. [42,43] and da Luz et al. [35] conducted 6-week follow-ups and found that patients with NSCLBP in the Pilates group exhibited improvements in fear of movement, quality of life, and degree of recovery; further, these improvements were maintained 6 months after training. Additionally, Gökmen et al. [46] conducted a three-month follow-up and determined that the Pilates training more effectively improved the general and mental health of CLBP patients than core stability–based home training. Cruz-Diaz et al. [36] conducted a 12-week study with mat Pilates and apparatus Pilates groups compared to a no-exercise group; significant improvements were observed in transversus abdominis activation and kinesiophobia during and after training in the Pilates groups. Batibay et al. [37] indicated that there were significant improvements in quality of life, depression, physical function, and core muscle thickness in patients after 8 weeks of Pilates training and home training, with patients who implemented Pilates training showing greater improvement in all parameters. Finally, Baskan et al. [38] determined that patients who underwent Pilates training exhibited significant improvements in muscle strength, lung function, disability levels, and balance after 8 weeks of training. In these RCTs, compliance was high, and no adverse outcomes were observed at follow-up [32,33,35-43,45,46]. These RCTs all indicated that Pilates training is a beneficial option for CLBP patients in terms of muscle strength, muscle size, physical function, balance, and recovery. These changes in balance and strength associated with Pilates training have beneficial effects on pain and function in CLBP patients, reducing the likelihood of disability and improving the quality of life in CLBP patients.
This study has some limitations. First, the methodological quality and risk of bias of the evaluated studies should be considered. Unlike previous studies, we relaxed the inclusion criteria, and some of the lower-quality studies were included, which may have contributed to inaccurate results in the corresponding analysis. Second, the population characteristics were not strictly restricted in our analysis, and sex and ethnicity were not described and analyzed in detail in the included studies; this may have had an overall impact on the interpretation of heterogeneity. Third, for the comparison of the ODI outcome of Pilates training with minimal intervention, we chose not to report the combined effect size for this outcome to avoid misleading results, as only two RCTs reported this outcome. Therefore, the results of this study may have been biased. Fourth, long-term Pilates training outcomes were not included in our analyses; these were excluded because most studies did not report this information and conducting a combined analysis may have led to inaccurate results. Despite the limitations of this study, few studies have examined the short- and medium-term effects of pain and disability in CLBP patients who underwent Pilates training. Therefore, the results of this systematic review and meta-analysis may assist medical professionals in determining whether to choose Pilates training for treatment of CLBP.
Based on the results of this systematic review and meta-analysis it was determined that Pilates training statistically significantly improves both pain disability and outcome compared to the minimal intervention with clinical significance. In addition, although pain and disability improvements were reduced in the medium-term after Pilates training compared to that in the short-term after Pilates training, statistically significant improvements were still observed, especially for the disability index, which remained clinically significant. Thus, Pilates is an effective treatment modality for patients with CLBP. Nonetheless, it is important to note that these results may be biased due to differences in subject characteristics and interventions between studies alongside the small number of high-quality studies available. Therefore, additional RCTs are required to overcome these limitations.