1.
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY. European guidance for the diagnosis and management of osteoporosis in postmenopausal women.
Osteoporos Int. 2008; 19: 399-428.


. Kanis JA., McCloskey EV., Johansson H., Cooper C., Rizzoli R., Reginster JY.. European guidance for the diagnosis and management of osteoporosis in postmenopausal women.
Osteoporos Int 2008;19:399-428. PMID:
10.1007/s00198-008-0560-z. PMID:
18266020.
2.
Reginster JY, Burlet N. Osteoporosis: a still increasing prevalence.
Bone. 2006; 38: 4-9.

. Reginster JY., Burlet N.. Osteoporosis: a still increasing prevalence.
Bone 2006;38:4-9. PMID:
10.1016/j.bone.2005.11.024. PMID:
16139579.
3.
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine.
J Bone Miner Res. 2014; 29: 2520-6.

Wright NC., Looker AC., Saag KG., Curtis JR., Delzell ES., Randall S., Dawson-Hughes B.. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine.
J Bone Miner Res 2014;29:2520-6. PMID:
10.1002/jbmr.2269. PMID:
24771492.
4.
Mithal A, Dhingra V, Lau E. The Asian audit: epidemiology, costs and burden of osteoporosis in Asia. 2009.
Mithal A., Dhingra V., Lau E.. The Asian audit: epidemiology, costs and burden of osteoporosis in Asia 2009.
5.
Choi YJ, Oh HJ, Kim DJ, Lee Y, Chung YS. The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: the Korea National Health and Nutrition Examination Survey 2008-2009.
J Bone Miner Res. 2012; 27: 1879-86.

. Choi YJ., Oh HJ., Kim DJ., Lee Y., Chung YS.. The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: the Korea National Health and Nutrition Examination Survey 2008-2009.
J Bone Miner Res 2012;27:1879-86. PMID:
10.1002/jbmr.1635. PMID:
22532494.
6.
Korea Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3). Ministry of Health and Welfare. 2009.
Korea Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3). Ministry of Health and Welfare. 2009.
7.
Oh EG, Yoo JY, Lee JE, Hyun SS, Ko IS, Chu SH. Effects of a three-month therapeutic lifestyle modification program to improve bone health in postmenopausal Korean women in a rural community: a randomized controlled trial.
Res Nurs Health. 2014; 37: 292-301.

. Oh EG., Yoo JY., Lee JE., Hyun SS., Ko IS., Chu SH.. Effects of a three-month therapeutic lifestyle modification program to improve bone health in postmenopausal Korean women in a rural community: a randomized controlled trial.
Res Nurs Health 2014;37:292-301. PMID:
10.1002/nur.21608. PMID:
24976566.
8.
Fleg JL. Aerobic exercise in the elderly: a key to successful aging. Discov Med. 2012; 13: 223-8.
. Fleg JL.. Aerobic exercise in the elderly: a key to successful aging.
Discov Med 2012;13:223-8. PMID:
22463798.
9.
Palombaro KM, Black JD, Buchbinder R, Jette DU. Effectiveness of exercise for managing osteoporosis in women postmenopause.
Phys Ther. 2013; 93: 1021-5.


. Palombaro KM., Black JD., Buchbinder R., Jette DU.. Effectiveness of exercise for managing osteoporosis in women postmenopause.
Phys Ther 2013;93:1021-5. PMID:
10.2522/ptj.20110476. PMID:
23704034.
10.
Zehnacker CH, Bemis-Dougherty A. Effect of weighted exercises on bone mineral density in post menopausal women. A systematic review.
J Geriatr Phys Ther. 2007; 30: 79-88.

. Zehnacker CH., Bemis-Dougherty A.. Effect of weighted exercises on bone mineral density in post menopausal women. A systematic review.
J Geriatr Phys Ther 2007;30:79-88. PMID:
10.1519/00139143-200708000-00007. PMID:
18171491.
11.
Lester ME, Urso ML, Evans RK, Pierce JR, Spiering BA, Maresh CM, Hatfield DL, Kraemer WJ, Nindl BC. Influence of exercise mode and osteogenic index on bone biomarker responses during short-term physical training. Bone. 2009; 45: 768-76.

Lester ME., Urso ML., Evans RK., Pierce JR., Spiering BA., Maresh CM., Hatfield DL., Kraemer WJ., Nindl BC.. Influence of exercise mode and osteogenic index on bone biomarker responses during short-term physical training.
Bone 2009;45:768-76. PMID:
10.1016/j.bone.2009.06.001. PMID:
19520194.
12.
Marques EA, Wanderley F, Machado L, Sousa F, Viana JL, Moreira-Gon├¦alves D, Moreira P, Mota J, Carvalho J. Effects of resistance and aerobic exercise on physical function, bone mineral density, OPG and RANKL in older women.
Exp Gerontol. 2011; 46: 524-32.

Marques EA., Wanderley F., Machado L., Sousa F., Viana JL., Moreira-Gon├¦alves D., Moreira P., Mota J., Carvalho J.. Effects of resistance and aerobic exercise on physical function, bone mineral density, OPG and RANKL in older women.
Exp Gerontol 2011;46:524-32. PMID:
10.1016/j.exger.2011.02.005. PMID:
21316442.
13.
Jeon YJ, Kim JW, Park JS. Factors associated with the treatment of osteoporosis in Korean postmenopausal women.
Women Health. 2014; 54: 48-60.

. Jeon YJ., Kim JW., Park JS.. Factors associated with the treatment of osteoporosis in Korean postmenopausal women.
Women Health 2014;54:48-60. PMID:
10.1080/03630242.2013.862896. PMID:
24219835.
14.
Kim KZ, Shin A, Lee J, Myung SK, Kim J. The beneficial effect of leisure-time physical activity on bone mineral density in pre-and postmenopausal women.
Calcif Tissue Int. 2012; 91: 178- 85.


. Kim KZ., Shin A., Lee J., Myung SK., Kim J.. The beneficial effect of leisure-time physical activity on bone mineral density in pre-and postmenopausal women.
Calcif Tissue Int 2012;91:178-85. PMID:
10.1007/s00223-012-9624-3. PMID:
22766920.
15.
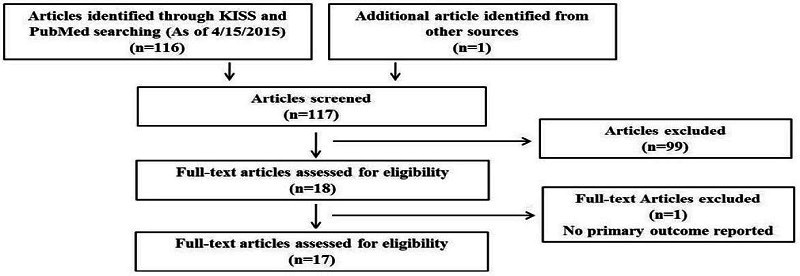
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
Int J Surg. 2010; 8: 336-41.

. Moher D., Liberati A., Tetzlaff J., Altman DG.. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
Int J Surg 2010;8:336-41. PMID:
10.1016/j.ijsu.2010.02.007. PMID:
20171303.
16.
Sung C, Yun M, Lee J, Kim M, Lee H. Effects of soy isoflavone supplementation and exercise on bone mineral density and urinary deoxypyridinoline in postmenopausal women. J Nutr and Health. 2004; 37: 291-301
. Sung C., Yun M., Lee J., Kim M., Lee H.. Effects of soy isoflavone supplementation and exercise on bone mineral density and urinary deoxypyridinoline in postmenopausal women.
J Nutr and Health 2004;37:291-301.
17.
Cho S. Changes of physical fitness and bone density following to swimming and resistance training in postmenopausal women.
J Sport and Leisure Studies. 2003; 19: 1435-44.

. Cho S.. Changes of physical fitness and bone density following to swimming and resistance training in postmenopausal women.
J Sport and Leisure Studies 2003;19:1435-44.
18.
Kim Y, Kang H, Jang J. The effect of weight bearing exercise on bone mineral density of postmenopausal womenŌĆÖs femoral and lumbar spine. Exer Sci. 1999; 8: 83-96.
. Kim Y., Kang H., Jang J.. The effect of weight bearing exercise on bone mineral density of postmenopausal womenŌĆÖs femoral and lumbar spine.
Exer Sci 1999;8:83-96.
19.
Ahn Y. Effect of participation in hata yoga and gate ball and weight-training on bone mineral density in postmenopausal women. Korean J Phy Edu. 2002; 41: 459-66.
. Ahn Y.. Effect of participation in hata yoga and gate ball and weight-training on bone mineral density in postmenopausal women.
Korean J Phy Edu 2002;41:459-66.
20.
Kim Y, Yoon Y. Effects of aerobic exercise on bone mineral density and lipid in postmenopausal women. J Korean Sports Med. 1999; 17: 385-94.
. Kim Y., Yoon Y.. Effects of aerobic exercise on bone mineral density and lipid in postmenopausal women.
J Korean Sports Med 1999;17:385-94.
21.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 ed. Chichester, United Kingdom. John Wiley & Sons Ltd. 2011.
Higgins J., Green S.Cochrane handbook for systematic reviews of interventions. Version 5.1.0 ed. Chichester. United Kingdom: John Wiley & Sons Ltd. 2011.
22.
Byeon J, Jeong S, Byeong J, Park S. Effects of 12 weeks the combined exercise program on the bone mineral density and isokinetic function of knee joint in the elderly women. Korean J Phy Edu. 2010; 49: 431-44.
. Byeon J., Jeong S., Byeong J., Park S.. Effects of 12 weeks the combined exercise program on the bone mineral density and isokinetic function of knee joint in the elderly women.
Korean J Phy Edu 2010;49:431-44.
23.
Byeon J, An G, Goong S, Park S, Seo J. Effects of the combined exercise program including step aerobics on bone mineral density and sex hormone in the elderly women. Korean J Phy Edu. 2009; 48: 411-20.
. Byeon J., An G., Goong S., Park S., Seo J.. Effects of the combined exercise program including step aerobics on bone mineral density and sex hormone in the elderly women.
Korean J Phy Edu 2009;48:411-20.
24.
Choi P. Long-term combined exercise has effect on regional bone mineral density and cardiovascular disease risk factors of the elderly with osteoporosis. J Korean Gerontol Soc. 2011; 31: 355-69.
. Choi P.. Long-term combined exercise has effect on regional bone mineral density and cardiovascular disease risk factors of the elderly with osteoporosis.
J Korean Gerontol Soc 2011;31:355-69.
25.
Choi E, Lee S. The effect of postmenopausal program of osteoporosis protection exercise on the density of bone and the improvement of physical fitness of middle-age women. Korean J Phy Edu. 2003; 42: 727-34.
. Choi E., Lee S.. The effect of postmenopausal program of osteoporosis protection exercise on the density of bone and the improvement of physical fitness of middle-age women.
Korean J Phy Edu 2003;42:727-34.
26.
Jee Y, Yoon K, Byun J, Kim M. The effects of exercise on bone mineral density and relating variables of elderly women with osteoporosis during taking the Alendronate®. J Sport and Leisure Studies. 2003; 9: 1455-66.
. Jee Y., Yoon K., Byun J., Kim M.. The effects of exercise on bone mineral density and relating variables of elderly women with osteoporosis during taking the Alendronate®.
J Sport and Leisure Studies 2003;9:1455-66.
27.
Kim E. The effect of combined exercise program on lumbar and femur neck bone mineral density and SOD, CAT, MDA activities in hysterectomy women.
Exer Sci. 2009; 18: 105-14.

. Kim E.. The effect of combined exercise program on lumbar and femur neck bone mineral density and SOD, CAT, MDA activities in hysterectomy women.
Exer Sci 2009;18:105-14. PMID:
10.15857/ksep.2009.18.1.105.
28.
Park H, Kim KJ, Komatsu T, Park SK, Mutoh Y. Effect of combined exercise training on bone, body balance, and gait ability: a randomized controlled study in community-dwelling elderly women.
J Bone Miner Metab. 2008; 26: 254-9.


. Park H., Kim KJ., Komatsu T., Park SK., Mutoh Y.. Effect of combined exercise training on bone, body balance, and gait ability: a randomized controlled study in community-dwelling elderly women.
J Bone Miner Metab 2008;26:254-9. PMID:
10.1007/s00774-007-0819-z. PMID:
18470666.
29.
Park S. The effects of exercise for preventing fall on postural sway, BMD and gait ability in elderly women. Korean J Phy Edu. 2002; 41: 583-94.
. Park S.. The effects of exercise for preventing fall on postural sway, BMD and gait ability in elderly women.
Korean J Phy Edu 2002;41:583-94.
30.
Kim Y, Jeong I. Effects of long term aerobic dance training on bone mineral density in postmenopausal women.
J Sport and Leisure Studie. 2004; 22: 369-78.

. Kim Y., Jeong I.. Effects of long term aerobic dance training on bone mineral density in postmenopausal women.
J Sport and Leisure Studie 2004;22:369-78.
31.
Jung S, Park G, Jin Y, Cho S, Hong K. The effect of exercise and hormone supplementation on physical fitness, body composition, blood profiles, and bone mineral density in early stage postmenopausal women. Korean J Phy Edu. 1999; 35: 217-27.
. Jung S., Park G., Jin Y., Cho S., Hong K.. The effect of exercise and hormone supplementation on physical fitness, body composition, blood profiles, and bone mineral density in early stage postmenopausal women.
Korean J Phy Edu 1999;35:217-27.
32.
Park I. Effects of 12 weeks aerobic exercise on health-related physical fitness and bone density in elderly.
J Sport and Leisure Studies. 2004; 22: 459-69.

. Park I.. Effects of 12 weeks aerobic exercise on health-related physical fitness and bone density in elderly.
J Sport and Leisure Studies 2004;22:459-69.
33.
Kim A. Effects of muscle strengthening exercise with elastic band on physical fitness and bone mineral density in the elderly women. J Korea Sport Res. 2010; 21: 95-114.
. Kim A.. Effects of muscle strengthening exercise with elastic band on physical fitness and bone mineral density in the elderly women.
J Korea Sport Res 2010;21:95-114.
34.
G├│mez-Cabello A, Ara I, Gonz├Īlez-Ag├╝ero A, Casaj├║s JA, Vicente-Rodr├Łguez G. Effects of training on bone mass in older adults: a systematic review.
Sports Med. 2012; 42: 301-25.

. G├│mez-Cabello A., Ara I., Gonz├Īlez-Ag├╝ero A., Casaj├║s JA., Vicente-Rodr├Łguez G.. Effects of training on bone mass in older adults: a systematic review.
Sports Med 2012;42:301-25. PMID:
10.2165/11597670-000000000-00000. PMID:
22376192.
35.
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, et al. Exercise for preventing and treating osteoporosis in postmenopausal women.
Cochrane Database Syst Rev. 2011; 6.

. Howe TE., Shea B., Dawson LJ., Downie F., Murray A., Ross C., et al. Exercise for preventing and treating osteoporosis in postmenopausal women.
Cochrane Database Syst Rev 2011;6:333PMID:
10.1002/14651858.cd000333.pub2.
36.
Kelley GA, Kelley KS, Kohrt WM. Effects of ground and joint reaction force exercise on lumbar spine and femoral neck bone mineral density in postmenopausal women: a meta-analysis of randomized controlled trials.
BMC musculoskelet disord. 2012; 13: 177-96.


. Kelley GA., Kelley KS., Kohrt WM.. Effects of ground and joint reaction force exercise on lumbar spine and femoral neck bone mineral density in postmenopausal women: a meta-analysis of randomized controlled trials.
BMC musculoskelet disord 2012;13:177-96. PMID:
10.1186/1471-2474-13-177. PMID:
22992273.
37.
Kelley GA, Kelley KS, Tran ZV. Exercise and lumbar spine bone mineral density in postmenopausal women: a meta-analysis of individual patient data.
J Gerontol A Biol Sci Med Sci. 2002; 57: 599-604.


. Kelley GA., Kelley KS., Tran ZV.. Exercise and lumbar spine bone mineral density in postmenopausal women: a meta-analysis of individual patient data.
J Gerontol A Biol Sci Med Sci 2002;57:599-604. PMID:
10.1093/gerona/57.9.M599.
38.
Heaney RP. The bone-remodeling transient: implications for the interpretation of clinical studies of bone mass change.
J Bone Miner Res. 1994; 9: 1515-23.

. Heaney RP.. The bone-remodeling transient: implications for the interpretation of clinical studies of bone mass change.
J Bone Miner Res 1994;9:1515-23. PMID:
10.1002/jbmr.5650091003. PMID:
7817796.
39.
Kelley GA, Kelley KS. Exercise and bone mineral density at the femoral neck in postmenopausal women: a meta-analysis of controlled clinical trials with individual patient data.
Am J Obstet Gynecol. 2006; 194: 760-7.

. Kelley GA., Kelley KS.. Exercise and bone mineral density at the femoral neck in postmenopausal women: a meta-analysis of controlled clinical trials with individual patient data.
Am J Obstet Gynecol 2006;194:760-7. PMID:
10.1016/j.ajog.2005.09.006. PMID:
16522410.
40.
National Institutes of Health Consensus Development Panel on Osteoporosis, Prevention, Diagnosis, and Therapy.
NIH Consensus Statement. 2000.

National Institutes of Health Consensus Development Panel on Osteoporosis, Prevention, Diagnosis, and Therapy. NIH Consensus Statement. 2000.
41.
Kemmler W, von Stengel S. Dose-response effect of exercise frequency on bone mineral density in post-menopausal, osteopenic women.
Scand J Med Sci Sports. 2014; 24: 526-34.

. Kemmler W., von Stengel S.. Dose-response effect of exercise frequency on bone mineral density in post-menopausal, osteopenic women.
Scand J Med Sci Sports 2014;24:526-34. PMID:
10.1111/sms.12024. PMID:
23190199.
42.
McNeely E. Training to Improve Bone Density in Adults: A Review and Recommendations by U.S Sports Academy. The Sport Journal. 2010.
McNeely E.. Training to Improve Bone Density in Adults: A Review and Recommendations by U.S Sports Academy.
The Sport Journal 2010.
43.
Turner CH, Robling AG. Mechanisms by which exercise improves bone strength.
J Bone Miner Metab. 2005; 23: 16-22.


. Turner CH., Robling AG.. Mechanisms by which exercise improves bone strength.
J Bone Miner Metab 2005;23:16-22. PMID:
10.1007/BF03026318. PMID:
15984409.
44.
Kelley GA, Kelley KS, Tran ZV. Resistance training and bone mineral density in women: a meta-analysis of controlled trials.
Am J Phys Med Rehabil. 2001; 80: 65-77.

. Kelley GA., Kelley KS., Tran ZV.. Resistance training and bone mineral density in women: a meta-analysis of controlled trials.
Am J Phys Med Rehabil 2001;80:65-77. PMID:
10.1097/00002060-200101000-00017. PMID:
11138958.
45.
Moreira LD, Oliveira ML, Lirani-Galv├Żo AP, Marin-Mio RV, Santos RN, Lazaretti-Castro M. Physical exercise and osteoporosis: effects of different types of exercises on bone and physical function of postmenopausal women.
Arq Bras Endocrinol Metabol. 2014; 58: 514-22.


. Moreira LD., Oliveira ML., Lirani-Galv├Żo AP., Marin-Mio RV., Santos RN., Lazaretti-Castro M.. Physical exercise and osteoporosis: effects of different types of exercises on bone and physical function of postmenopausal women.
Arq Bras Endocrinol Metabol 2014;58:514-22. PMID:
10.1590/0004-2730000003374. PMID:
25166042.
46.
Martyn-St James M, Carroll S. A meta-analysis of impact exercise on postmenopausal bone loss: the case for mixed loading exercise programmes.
Br J Sports Med. 2009; 43: 898-908.

. Martyn-St James M., Carroll S.. A meta-analysis of impact exercise on postmenopausal bone loss: the case for mixed loading exercise programmes.
Br J Sports Med 2009;43:898-908. PMID:
10.1136/bjsm.2008.052704. PMID:
18981037.
47.
Floras JS, Notarius CF, Harvey PJ. Exercise training--not a class effect: blood pressure more buoyant after swimming than walking.
J Hypertens. 2006; 24: 269-72.

. Floras JS., Notarius CF., Harvey PJ.. Exercise training--not a class effect: blood pressure more buoyant after swimming than walking.
J Hypertens 2006;24:269-72. PMID:
10.1097/01.hjh.0000202814.79964.84. PMID:
16508569.
48.
Guadalupe-Grau A, Fuentes T, Guerra B, Calbet JA. Exercise and bone mass in adults.
Sports Med. 2009; 39: 439-68.

. Guadalupe-Grau A., Fuentes T., Guerra B., Calbet JA.. Exercise and bone mass in adults.
Sports Med 2009;39:439-68. PMID:
10.2165/00007256-200939060-00002. PMID:
19453205.
49.
Aldahr MHS. Bone Mineral Status Response to Aerobic Versus Resistance Exercise Training in Postmenopausal Women. World Appl Sci J.2012; 16: 806-13. Retrived from http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.389.5529&rep=rep1&type=pdf.
. Aldahr MHS.. Bone Mineral Status Response to Aerobic Versus Resistance Exercise Training in Postmenopausal Women.
World Appl Sci J 2012 16:806-13. Retrived from
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.389.5529&rep=rep1&type=pdf.
50.
Warriner AH, Patkar NM, Curtis JR, Delzell E, Gary L, Kilgore M, Saag K. Which fractures are most attributable to osteoporosis?
J Clin Epidemiol. 2011; 64: 46-53.

Warriner AH., Patkar NM., Curtis JR., Delzell E., Gary L., Kilgore M., Saag K.. Which fractures are most attributable to osteoporosis?
J Clin Epidemiol 2011;64:46-53. PMID:
10.1016/j.jclinepi.2010.07.007. PMID:
21130353.