|
 |
- Search
| Phys Act Nutr > Volume 28(1); 2024 > Article |
|
Abstract
[Purpose]
This narrative review evaluated the impact of exercise on gait and cognitive functions in patients with Parkinson’s disease (PD), focusing on prefrontal cortical (PFC) activation assessed using near-infrared spectroscopy (NIRS).
[Methods]
A literature search was conducted in the PubMed and Web of Science databases using keywords such as “Parkinson’s disease,” “gait,” “cognitive functions,” “exercise,” and “NIRS,” focusing on publications from the last decade. Studies measuring PFC activity using NIRS during gait tasks in patients with PD were selected.
[Results]
The review indicated that patients with PD demonstrate increased PFC activity during gait tasks compared to healthy controls, suggesting a greater cognitive demand for movement control. Exercise has been shown to enhance neural efficiency, thus improving gait and cognitive functions.
[Conclusion]
Exercise is crucial for improving gait and cognitive functions in patients with PD through increased PFC activation. This emphasizes the importance of incorporating exercise into PD management plans and highlights the need for further studies on its long-term effects and the neurobiological mechanisms underlying its benefits, with the aim of optimizing therapeutic strategies and improving patients’ quality of life.
As South Korea rapidly progresses into a super-aged society, the prevalence of neurodegenerative disorders such as Parkinson’s disease (PD) is increasing, challenging both research and healthcare paradigms. A comprehensive analysis utilizing data from the Korean National Health Insurance Service underscores this trend, revealing a continuous increase in PD incidence from 2007 to 2018, with the disease incidence notably rising with age, peaking at 80 years [1]. This demographic shift highlights the need to address conditions characterized by a complex interplay of motor and cognitive dysfunction that critically undermine activities of daily living and independence [1,2]. PD is characterized by classic motor symptoms, such as tremors, rigidity, bradykinesia (slow movement), and postural instability, as well as cognitive impairments in executive functions and gait control, all of which are essential for maintaining a sustainable quality of life [3,4].
The interplay between motor and cognitive declines in PD delineates a complex clinical landscape that significantly deteriorates patients’ quality of life, necessitating targeted interventions for managing both the physical and cognitive domains of the disease [5-7]. At the core of PD’s neurobiology is the degeneration of dopamine-producing neurons in the substantia nigra, resulting in diminished signaling crucial for movement control [8] and disruption of various neural pathways and neurotransmitter systems, contributing to the wide range of PD symptoms experienced by patients [9-11]. This complex neurobiological foundation underscores the need for a profound understanding of the mechanisms underlying PD to develop holistic care strategies to manage diverse symptomatologies and enhance patient well-being [12,13].
Gait control, a fundamental aspect of mobility, significantly affects the autonomy and safety of patients with PD. Gait disturbances in PD are characterized by shuffling steps, freezing episodes, and a higher risk of falls, reflecting not only the progression of the disease but also its cognitive implications. Notably, deterioration in gait control is closely linked to cognitive decline, particularly in executive functions. This link highlights a bidirectional relationship in which impairments in each domain exacerbate impairments in others, underscoring the intertwined nature of motor and cognitive functions in PD. Recent studies have provided compelling evidence for this complex relationship. Research conducted on gait patterns in patients with PD, with and without cognitive impairment, revealed that those with cognitive impairment exhibit significant reductions in gait speed, step length, and stride length [14]. Furthermore, specific cognitive functions, such as “registration,” “attention/calculation,” and “visuospatial function,” were found to be significantly associated with these gait parameters, demonstrating the profound impact of cognitive abilities on gait control [14,15]. Similarly, another study demonstrated that mild cognitive impairment in patients with PD is associated with poor gait performance, particularly affecting gait velocity and stride length. This association is most pronounced for attention and frontal-executive functions, reinforcing the pivotal role of cognitive processes in gait regulation [16]. Considering these challenges, it is imperative to explore interventions that can simultaneously address the interconnected aspects of PD.
In response to the growing attention paid to targeted interventions, including exercise, this review will rigorously examine how gait control abilities are compromised in PD compared to those of healthy individuals, delving into the associated neural activity in the prefrontal cortex, measured using near-infrared spectroscopy (NIRS). The questions guiding this inquiry are focused on distinguishing gait control abilities between patients with PD and healthy controls in relation to neural activity, understanding how PD progression affects gait control and the corresponding neural activities, exploring the influence of increased demands on the prefrontal cortex on gait control in PD, and investigating whether structured exercise programs can enhance prefrontal cortex efficiency and, in turn, gait control in patients with PD.
Numerous studies have suggested that exercise can be a potent non-pharmacological intervention to improve both motor and cognitive functions in PD, potentially mediated by increased neural efficiency in the prefrontal cortex, a brain region critical for executive functions. NIRS is a noninvasive method for observing these neural changes, thereby providing a window into the underlying brain mechanisms affected by exercise. This review aims to synthesize findings from diverse original studies and critically assess the consistencies and discrepancies to outline future research pathways. By highlighting the role of NIRS in evaluating PD’s impact on gait control, executive functions, and frontal lobe activity, we sought to deepen our understanding of PD and inform the development of effective non-pharmacological interventions to improve the quality of life of patients with PD.
The current study adopted a narrative review methodology to explore the broad spectrum of interventions that influence prefrontal cortical (PFC) activation and their effects on gait and cognitive function in patients with PD. This includes a particular focus on exercise, assessed using NIRS during gait tasks, while also considering the comparative and contextual effects of dopaminergic medication. The literature search was conducted using specific keywords such as “Parkinson’s disease,” “gait,” “cognitive functions,” “exercise,” and “NIRS” in the PubMed and Web of Science databases for articles published in the last decade.
The inclusion and classification criteria for the articles obtained through the database searches were as follows.
1. Studies involving patients with PD.
2. Research measuring PFC activation using NIRS during gait tasks.
3. Studies that assessed PFC activation using NIRS during gait tasks while simultaneously performing cognitive tasks.
4. Research evaluating the influence of interventions, including medication or exercise, on gait control ability and measuring PFC activation using NIRS during tasks.
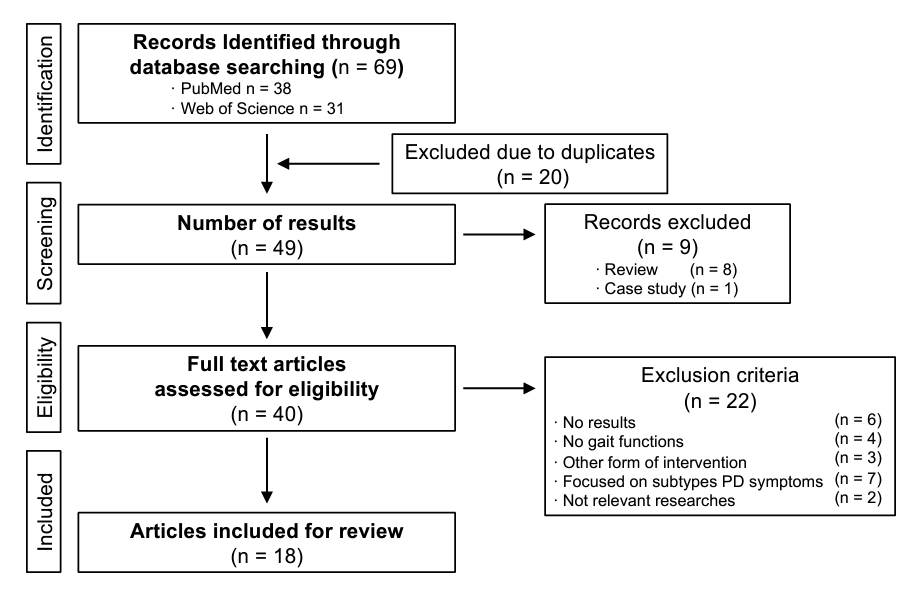
To maintain focus on original empirical research, articles in the form of reviews or commentaries were excluded from the selection process. In addition, 20 articles were excluded for the following reasons: 6 had no results pertinent to our review’s objectives, 4 did not measure gait function, 3 involved other forms of intervention not relevant to our focus, 7 focused on subtypes of PD symptoms that were not within our scope, and 2 were deemed not relevant to the research questions. After a comprehensive screening and eligibility assessment, 18 articles were selected for inclusion in this review (Figure 1). The aim of this narrative review was to synthesize current findings and insights into the role of exercise in enhancing gait and cognitive functions in patients with PD, emphasizing the neurophysiological measurements obtained using NIRS.
Following the pioneering work of Nieuwhof et al. (2016), which demonstrated the feasibility of monitoring PFC activation in real-world settings using portable functional NIRS, several studies have emerged focusing on neural activity during walking in patients with PD (Table 1). These studies suggest that a significant cognitive burden is associated with motor control in patients with PD, where activities such as walking, turning, and dual-task walking elicit heightened cortical activation [17-21]. Notably, compared to healthy controls, patients with PD have been shown to exhibit increased prefrontal and frontal cortical activation during walking and complex gait tasks [18,19]. Stuart et al. (2019) further demonstrated that PFC activity during walking and turning tasks distinctively differentiates patients with PD from both younger and older adults, emphasizing the augmented cognitive effort that patients with PD expend for motor control. This surge in neural activation may be interpreted as a compensatory response to the combined motor and cognitive challenges associated with PD. The use of prefrontal brain regions suggests that patients need extra cognitive resources to control movement, especially in conditions requiring gait adaptability and executive function engagement.
Regarding neural variability and cognitive-motor interference, several studies have explored the increased neural variability in the prefrontal cortex and the neural substrates of cognitive-motor interference [22,23]. These findings suggest that the observed neural variability in the prefrontal cortex of patients with PD represents a delicate balance between neural flexibility and stability, potentially affecting their ability to manage cognitive-motor interference during walking. Such variability may serve as an adaptive mechanism for maintaining gait control despite PD-related motor and cognitive deficits.
Furthermore, research focusing on cortical activation patterns in relation to gait adaptability, hemodynamic responses, and obstacle negotiation offers additional insights [24-26]. For instance, Pelicionie et al. (2022) examined how patients with PD adjust their gait in response to varying walking conditions, such as changing speeds or avoiding obstacles, and found that these patients exhibit altered cortical activation, particularly in brain regions associated with motor planning and execution, during gait adaptability tasks. This alteration suggests a need for patients with PD to exert additional cognitive efforts to modify their gait in dynamic environments, potentially reflecting compensatory neural mechanisms for motor deficits. Moreover, Wang et al. (2023) utilized functional NIRS to measure frontal hemodynamic patterns in patients with PD performing the Timed-Up-and-Go test, revealing distinctive frontal hemodynamic patterns in these patients compared to controls, characterized by differences in oxygenation levels in the prefrontal cortex. These differences indicate that patients with PD may utilize different neural circuits or employ more cognitive control to perform the same physical tasks as controls. Assad et al. (2022) further investigated the impact of disease severity on PFC activation during obstacle negotiation, a task requiring both cognitive planning and motor execution. Interestingly, they found that the association between disease severity and cortical activation is not linear, suggesting that individual variability in compensatory neural mechanisms can significantly influence how the disease manifests as cortical activity patterns.
In summary, these studies collectively emphasize the pivotal role of increased activity in the prefrontal and frontal cortices in managing gait and cognitive tasks in patients with PD, indicating a pronounced cognitive burden for motor control. They revealed a nuanced interplay among neural variability, flexibility, and compensatory mechanisms in gait control in patients with PD. While some studies have emphasized the involvement of the prefrontal cortex, others have pointed to broader neural network changes, including enhanced connectivity in the left parietal lobe. These findings elucidate the complex neural dynamics underlying gait control in PD and highlight the necessity for personalized interventions to effectively address the multifaceted nature of PD-related gait impairments.
This section describes research on the impact of various interventions, including dopaminergic therapy and exercise, on PFC activation during walking in individuals with PD. It delves into the neural mechanisms and implications of these interventions, highlighting their significance in enhancing cognitive and motor performance (Table 2).
Dopaminergic therapy, especially the administration of levodopa, is pivotal in enhancing PFC activation during walking tasks in patients with PD. Research has consistently demonstrated that levodopa significantly improves cognitive and motor performance in complex walking scenarios, such as dual-task walking and obstacle avoidance, by addressing dopaminergic deficits inherent to PD [28-30]. Specifically, Dagan et al. (2021) explored the effect of levodopa on PFC activation and examined its role within the framework of the levodopa overdose hypothesis. This hypothesis posits that while levodopa is crucial for symptom management in PD, its dosing requires meticulous calibration to mitigate potential adverse effects, such as motor and cognitive impairment [31,32]. The findings affirm the hypothesis, suggesting that although levodopa boosts cortical activity for improved executive function, dosage management is essential to mitigate overdosing risks, such as increased risk of falls or dyskinesia.
The dual function of levodopa in facilitating motor control and cognitive processing during walking tasks has been further elucidated. Orcioli-Silva et al. (2020) demonstrated that levodopa therapy aids prefrontal activation during dual-tasking walking, suggesting enhanced functional mobility. This emphasizes levodopa’s utility in improving the quality of life of patients with PD by ensuring better navigation through complex environments via augmented cognitive-motor integration. Furthermore, research on gait improvements and obstacle avoidance has revealed that levodopa increases PFC activation, promoting efficient motor control and reducing the cognitive load associated with complex walking tasks [30].
The collective findings from these studies elucidate the underlying mechanism by which dopaminergic therapy, particularly levodopa, enhances PFC activation, thereby ameliorating both cognitive and motor aspects of walking in patients with PD. The principal mechanism seems to be the medication’s ability to counteract PD-related dopaminergic deficits, enhancing executive function and attention during walking. These insights suggest that the optimal dosing of dopaminergic therapy can significantly improve gait control and cognitive function, potentially elevating the quality of life of patients with PD. However, this study also cautions against the potential risks of overdose and emphasizes the need for personalized medication management to maximize benefits while minimizing adverse effects.
In light of the concerns regarding the adverse effects of dopaminergic therapy, the exploration of non-pharmacological interventions, such as exercise, has become highly relevant. Exercise emerges as a complementary and alternative therapeutic strategy with minimal side effects [33,34], capable of enhancing PFC activation [35-37] thereby improving cognitive and motor performance in patients with PD. Furthermore, recent studies have investigated the effect of intervention type on PFC activation during walking in patients with PD, revealing a compelling argument for exercise with cognitive or neuromodulatory interventions. These studies collectively focused on how different intervention strategies modulate the neural mechanisms underlying motor and cognitive functions in PD, suggesting a path toward more effective and personalized therapeutic approaches [18,38-40].
The essential role of physical exercise in modulating brain activity and improving motor function in patients with PD is evident in several studies. For instance, Hoang et al. (2021) demonstrated that an intensive, multidisciplinary exercise-based training program is effective in reducing PFC activity during typical walking tasks. This finding suggests that exercise alone can enhance the automaticity of walking in patients with PD, reducing the cognitive load required for basic gait tasks and potentially freeing up executive resources for more complex motor functions. The inherent benefits of exercise highlight its importance as a fundamental component of PD management, promoting more effective prefrontal plasticity and improving gait performance.
Building upon the benefits of exercise in PD, many researchers have attempted to integrate cognitive or neuromodulatory interventions to further enhance prefrontal plasticity and improve overall therapeutic outcomes [38,39]. Interestingly, Maidan et al. (2018) examined the effects of a treadmill, with and without the addition of virtual reality, and revealed how adding a cognitive challenge can modify PFC activation not only by reducing its magnitude but also by affecting its lateralization and significantly impacting fall rates. These findings suggest that targeting motor and cognitive functions simultaneously can produce distinct neural and functional benefits, enhance plasticity, and potentially reduce the risk of falls in patients with PD. Moreover, Conceição et al. (2021) examined the synergistic effects of combining aerobic exercise with transcranial direct current stimulation (tDCS) over the prefrontal cortex and focused on the potential of tDCS to amplify the cognitive and motor benefits of physical exercise. They found that this combination led to immediate improvements in gait variability, processing speed, and executive control, along with an increase in PFC activity. These results also highlight the added value of neuromodulation in conjunction with exercise, indicating a potentiating effect on both cognitive function and gait control in patients with PD.
This narrative review elucidates the pivotal role of exercise in modulating PFC activity in patients with PD, which is a critical factor in the management of both gait control and executive functions. The increased reliance on PFC activation in patients with PD, as indicated in the reviewed studies, suggests an elevated cognitive demand for motor control, necessitating additional cognitive resources [19,20,41]. These findings emphasize the importance of exercise as a fundamental component of therapeutic strategies to improve the quality of life of patients with PD. Moreover, the variability in response to exercise intervention points to the need for personalized approaches to manage PD, considering individual differences in disease progression, baseline motor and cognitive abilities, and personal preference [33].
Emerging research has revealed a critical adaptive response in the prefrontal cortex of patients with PD, characterized by increased cortical activation during gait control. This suggests a compensatory mechanism to counterbalance the neurodegenerative effects of the disease. Dopaminergic therapy, notably levodopa, enhances cortical activation during walking tasks, thereby improving cognitive and motor performance by counteracting dopaminergic deficits [28,30]. This increase in cortical activity reflects a compensatory attempt to maintain motor control and cognitive processing efficiency despite the inherent neural inefficiencies of PD. Furthermore, exercise interventions have emerged as a pivotal non-pharmacological approach that enhances cortical activation, particularly in the dorsolateral prefrontal cortex, and consequently improves cognitive and motor functions [35-37,42]. For instance, an intensive, multidisciplinary exercise program has demonstrated effectiveness in reducing the cognitive load required for gait tasks [40], suggesting the potential for exercise to bolster the automaticity of walking and preserve the functional reserve in patients with PD.
Further analysis of the association between cognitive impairment and gait control in patients with PD reveals a complex, bidirectional interplay, where impairments in one domain can exacerbate challenges in others. Studies have shown that cognitive deficits, particularly in executive function and attention, significantly contribute to the complexity of gait disturbance, increasing the cognitive load during motor tasks such as walking [14,15]. This heightened demand for cognitive resources necessitates an increased PFC activation, indicative of a compensatory mechanism for maintaining gait stability [18-20]. Conversely, efforts to manage gait control in patients with PD can strain cognitive resources, further impairing cognitive functions and creating a cycle that accelerates symptom progression [26]. Understanding this bidirectional relationship is crucial for developing PD management strategies that simultaneously target cognitive functions and gait control.
Although the short-term benefits of exercise are well-documented, the sustainability of these effects over time remains underexplored. Future research should delve into longitudinal studies to assess the enduring impact of exercise on PFC activation and consequent improvements in gait and cognitive function in patients with PD. In addition, comparative studies examining the effectiveness of different exercise modalities could provide critical insights into optimizing exercise prescriptions for patients with PD, potentially leading to tailored exercise programs that cater to the unique needs of individual patients [33,34,43].
Although this review sheds light on the role of enhanced neural efficiency, the specific pathways involved in these processes remain unclear. Further exploration is warranted into the underlying neurobiological mechanisms through which exercise exerts its beneficial effects on the prefrontal cortex and, consequently, on motor and cognitive functions in PD. A deeper understanding of these neurobiological mechanisms could pave the way for the development of targeted interventions that effectively leverage the neuroprotective and neurorestorative potentials of exercise [23,44]
This narrative review emphasizes the importance of exercise in improving PFC activation and consequently enhancing gait and cognitive function in patients with PD. It advocates for the integration of exercise into comprehensive PD management plans, tailored to the individual needs of patients. The findings from the current review call for future research to focus on the long-term effects of exercise, comparative efficacy of different exercise types, and elucidation of the neurobiological mechanisms underlying the beneficial effects of exercise. Such endeavors will not only enhance our understanding of PD but also contribute to the development of more effective, personalized therapeutic strategies for managing this complex condition, ultimately improving the quality of life of patients with PD.
Acknowledgments
This study was supported by Incheon National University Research Grant in 2019. The author declares no conflicts of interest related to the work in this manuscript.
Table 1.
Neuroimaging studies on gait and cognitive function in Parkinson's disease.
Table 2.
Interventions impacting prefrontal cortical activity and gait performance in Parkinson's disease.
REFERENCES
1. Kang SH, Moon SJ, Kang M, Chung SJ, Cho GJ, Koh SB. Incidence of Parkinson’s disease and modifiable risk factors in Korean population: a longitudinal follow-up study of a nationwide cohort. Front Aging Neurosci 2023;15:1094778.



2. Park JH, Kim DH, Kwon DY, Choi M, Kim S, Jung JH, Han K, Park YG. Trends in the incidence and prevalence of Parkinson’s disease in Korea: a nationwide, population-based study. BMC Geriatr 2019;19:320.




3. Armstrong MJ, Okun MS. Diagnosis and treatment of Parkinson disease: a review. JAMA 2020;323:548-60.


5. Kataoka H, Tanaka N, Eng M, Saeki K, Kiriyama T, Eura N, Ikeda M, Izumi T, Kitauti T, Furiya Y, Sugie K, Ikada Y, Ueno S. Risk of falling in Parkinson’s disease at the hoehn-yahr stage III. Eur Neurol 2011;66:298-304.



6. Nemanich ST, Duncan RP, Dibble LE, Cavanaugh JT, Ellis TD, Ford MP, Foreman KB, Earhart GM. Predictors of gait speeds and the relationship of gait speeds to falls in men and women with Parkinson disease. Parkinsons Dis 2013;2013:141720.




7. Caetano MJD, Lord SR, Allen NE, Song J, Paul SS, Canning CG, Menant JCC. Executive functioning, muscle power and reactive balance are major contributors to gait adaptability in people with Parkinson’s disease. Front Aging Neurosci 2019;11:154.



8. Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, Schrag AE, Lang AE. Parkinson disease. Nat Rev Dis Primers 2017;3:17013.



9. Muñoz A, Lopez-Lopez A, Labandeira CM, Labandeira-Garcia JL. Interactions between the serotonergic and other neurotransmitter systems in the basal ganglia: role in Parkinson’s disease and adverse effects of L-DOPA. Front Neuroanat 2020;14:26.


10. Bohnen NI, Yarnall AJ, Weil RS, Moro E, Moehle MS, Borghammer P, Bedard MA, Albin RL. Cholinergic system changes in Parkinson’s disease: emerging therapeutic approaches. Lancet Neurol 2022;21:381-92.



11. Bohnen NI, Albin RL. The cholinergic system and Parkinson disease. Behav Brain Res 2011;221:564-73.


12. van der Marck MA, Bloem BR. How to organize multispecialty care for patients with Parkinson’s disease. Parkinsonism Relat Disord 2014;20:S167-73.


13. Hammarlund CS, Andersson K, Andersson M, Nilsson MH, Hagell P. The significance of walking from the perspective of people with Parkinson’s disease. J Parkinsons Dis 2014;4:657-63.


14. Kim SM, Kim DH, Yang Y, Ha SW, Han JH. Gait Patterns in Parkinson’s disease with or without cognitive impairment. Dement Neurocogn Disord 2018;17:57-65.




15. Amboni M, Barone P, Iuppariello L, Lista I, Tranfaglia R, Fasano A, Picillo M, Vitale C, Santangelo G, Agosti V, Iavarone A, Sorrentino G. Gait patterns in Parkinsonian patients with or without mild cognitive impairment. Mov Disord 2012;27:1536-43.


16. Kang SH, Kim J, Lee J, Koh SB. Mild cognitive impairment is associated with poor gait performance in patients with Parkinson’s disease. Front Aging Neurosci 2022;14:1003595.



17. Nieuwhof F, Reelick MF, Maidan I, Mirelman A, Hausdorff JM, Rikkert MGMO, Bloem BR, Muthalib M, Claassen JAHR. Measuring prefrontal cortical activity during dual task walking in patients with Parkinson’s disease: feasibility of using a new portable fNIRS device. Pilot Feasibility Stud 2016;2:59.




18. Ranchet M, Hoang I, Cheminon M, Derollepot R, Devos H, Perrey S, Luauté J, Danaila T, Paire-Ficout L. Changes in prefrontal cortical activity during walking and cognitive functions among patients with Parkinson’s disease. Front Neurol 2020;11:601686.



19. Maidan I, Nieuwhof F, Bernad-Elazari H, Reelick MF, Bloem BR, Giladi N, Deutsch JE, Hausdorff JM, Claassen JAH, Mirelman A. The role of the frontal lobe in complex walking among patients with Parkinson’s disease and healthy older adults. Neurorehabil Neural Repair 2016;30:963-71.



20. Stuart S, Belluscio V, Quinn JF, Mancini M. Pre-frontal cortical activity during walking and turning is reliable and differentiates across young, older adults and people with Parkinson’s disease. Front Neurol 2019;10:536.



21. Liu YC, Yang YR, Yeh NC, Ku PH, Lu CF, Wang RY. Multiarea brain activation and gait deterioration during a cognitive and motor dual task in individuals with Parkinson disease. J Neurol Phys Ther 2022;46:260-9.


22. Al-Yahya E, Mahmoud W, Meester D, Esser P, Dawes H. Neural substrates of cognitive motor interference during walking; peripheral and central mechanisms. Front Hum Neurosci 2019;12:536.



23. Maidan I, Hacham R, Galperin I, Giladi N, Holtzer R, Hausdorff JM, Mirelman A. Neural variability in the prefrontal cortex as a reflection of neural flexibility and stability in patients with Parkinson disease. Neurology 2022;98:e839-47.


24. Wang Y, Yu N, Lu J, Zhang X, Wang J, Shu Z, Cheng Y, Zhu Z, Yu Y, Liu P, Han J, Wu J. Increased effective connectivity of the left parietal lobe during walking tasks in Parkinson’s disease. J Parkinsons Dis 2023;13:165-78.



25. Pelicioni PHS, Lord SR, Okubo Y, Menant JC. Cortical activation during gait adaptability in people with Parkinson’s disease. Gait Posture 2022;91:247-53.


26. Assad M, Galperin I, Giladi N, Mirelman A, Hausdorff JM, Maidan I. Disease severity and prefrontal cortex activation during obstacle negotiation among patients with Parkinson’s disease: is it all as expected? Parkinsonism Relat Disord 2022;101:20-6.


27. Tao P, Shao X, Dong Y, Adams R, Preston E, Liu Y, Han J. Functional near-infrared spectroscopy measures of frontal hemodynamic responses in Parkinson’s patients and controls performing the timed-up-and-go test. Behav Brain Res 2023;438:114219.


28. Dagan M, Herman T, Bernad-Elazari H, Gazit E, Maidan I, Giladi N, Mirelman A, Manor B, Hausdorff JM. Dopaminergic therapy and prefrontal activation during walking in individuals with Parkinson’s disease: does the levodopa overdose hypothesis extend to gait? J Neurol 2021;268:658-68.



29. Orcioli-Silva D, Vitório R, Nóbrega-Sousa P, Conceição NR da, Beretta VS, Lirani-Silva E, Gobbi LTB. Levodopa facilitates prefrontal cortex activation during dual task walking in Parkinson disease. Neurorehabil Neural Repair 2020;34:589-99.



30. Orcioli-Silva D, Vitório R, Nóbrega-Sousa P, Beretta VS, Conceição NR da, Oliveira AS, Pereira MP, Gobbi LTB. Cortical activity underlying gait improvements achieved with dopaminergic medication during usual walking and obstacle avoidance in Parkinson disease. Neurorehabil Neural Repair 2021;35:406-18.



31. Rinaldi D, Carolis LD, Ceriello F, Bianchini E, Pontieri FE. Levodopa/carbidopa intestinal gel for pain related to levodopa-induced motor complications in Parkinson’s disease. Neurol Sci 2022;43:4571-2.



32. Nyholm D, Jost WH. Levodopa-entacapone-carbidopa intestinal gel infusion in advanced Parkinson’s disease: real-world experience and practical guidance. Ther Adv Neurol Disord 2022;15:17562864221108018.




33. da Silva FC, Iop R da R, de Oliveira LC, Boll AM, de Alvarenga JGS, Filho PJBG, de Melo LMAB, Xavier AJ, da Silva R. Effects of physical exercise programs on cognitive function in Parkinson’s disease patients: a systematic review of randomized controlled trials of the last 10 years. PLoS One 2018;13:e0193113.



34. Zhang T, Liu W, Bai Q, Gao S. The therapeutic effects of yoga in people with Parkinson’s disease: a mini-review. Ann Med 2023;55:2294935.



35. Kujach S, Byun K, Hyodo K, Suwabe K, Fukuie T, Laskowski R, Dan I, Soya H. A transferable high-intensity intermittent exercise improves executive performance in association with dorsolateral prefrontal activation in young adults. Neuroimage 2018;169:117-25.


36. Byun K, Hyodo K, Suwabe K, Ochi G, Sakairi Y, Kato M, Dan I, Soya H. Positive effect of acute mild exercise on executive function via arousal-related prefrontal activations: an fNIRS study. Neuroimage 2014;98:336-45.


37. Hyodo K, Dan I, Suwabe K, Kyutoku Y, Yamada Y, Akahori M, Byun K, Kato M, Soya H. Acute moderate exercise enhances compensatory brain activation in older adults. Neurobiol Aging 2012;33:2621-32.


38. Maidan I, Nieuwhof F, Bernad-Elazari H, Bloem BR, Giladi N, Hausdorff JM, Claassen JAHR, Mirelman A. Evidence for differential effects of 2 forms of exercise on prefrontal plasticity during walking in Parkinson’s disease. Neurorehabil Neural Repair 2018;32:200-8.



39. Conceição NR, Gobbi LTB, Nóbrega-Sousa P, Orcioli-Silva D, Beretta VS, Lirani-Silva E, Okano AH, Vitório R. Aerobic exercise combined with transcranial direct current stimulation over the prefrontal cortex in Parkinson disease: effects on cortical activity, gait, and cognition. Neurorehabil Neural Repair 2021;35:717-28.



40. Hoang I, Ranchet M, Cheminon M, Derollepot R, Devos H, Perrey S, Luauté J, Danaila T, Paire-Ficout L. An intensive exercise-based training program reduces prefrontal activity during usual walking in patients with Parkinson’s disease. Clin Park Relat Disord 2021;6:100128.



41. Maidan I, Bernad-Elazari H, Giladi N, Hausdorff JM, Mirelman A. When is higher level cognitive control needed for locomotor tasks among patients with Parkinson’s disease? Brain Topogr 2017;30:531-8.



42. Robertson CV, Marino FE. A role for the prefrontal cortex in exercise tolerance and termination. J Appl Physiol 2016;120:464-6.


43. Kim R, Choi S, Kang N, Park K, Shin H, Lee H, Lee H, Jun JS, Jeon B, Byun K. Effects of high-intensity interval training and moderate-intensity continuous training on sarcopenia-related parameters in participants with Parkinson’s disease: a 24-week randomized pilot trial substudy. Parkinsonism Relat Disord 2023;117:105901.