Effect of exercise intervention using mobile healthcare on blood lipid level and health-related physical fitness in obese women: a randomized controlled trial
Article information
Abstract
[Purpose]
This study aimed to evaluate the effects of 12 weeks of non-face-to-face exercise intervention using mobile health (mHealth) on blood lipid levels and health-related physical fitness in obese women.
[Methods]
Thirty obese women (aged: 39.40 ± 11.07 years, percent body fat: 37.05 ± 5.15%) were enrolled, and all completed the study. Non-face-to-face exercises were performed for 12 weeks using a mHealth and smart tracker (Charge 4, Fitbit, USA). Participants were randomly assigned to an experimental (EXP) or control (CON) group. The 12-week exercise program using mHealth included resistance (twice a week for 60 min), aerobics (five times a week for 50 min), and flexibility (five times a week for 10 min).
[Results]
The results showed that high-density lipoprotein cholesterol (Post − Pre: 9.07 mg·dL-1, p < 0.001) and ratio of low-density to high-density lipoprotein cholesterol (Post − Pre: −0.71 mg·dL-1, p < 0.05) significantly changed during the intervention period in EXP. There were significant increases in sit-ups (Post − Pre: 7.73 numbers, p < 0.001), grip strength (Post − Pre: 2.92 kg, p < 0.001), and sit and reach (Post − Pre: 2.51 cm, p < 0.01) in EXP.
[Conclusion]
Non-face-to-face exercise using mHealth for 12 weeks improved blood lipid levels and health-related physical fitness; therefore, it can help improve compliance through self-monitoring and lifestyle changes by increasing physical activity.
INTRODUCTION
Obesity is an epidemic metabolic disease [1] and the third leading cause of death and a risk factor for various types of health problems worldwide [2-4]. The leading causes of the continuous increase in the prevalence of obesity are busy daily life, nutritional imbalance, and increased sedentary lifestyle [5]. Over third of adults worldwide suffer from obesity, and women have a higher obesity rate than men [3,6]. Obesity negatively affects low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), and triglyceride (TG) levels, thereby increasing the risk of metabolic syndrome and cardiovascular diseases (CVD) such as dyslipidemia, type 2 diabetes, and hypertension, leading to early death [3,7-10].
Various intervention methods have been developed to treat obesity; however, its worldwide prevalence has not decreased [11-14]. Drugs and surgical treatments effectively treat obesity but can cause limited and severe side effects [14]. Regular physical activity (PA) is one of the methods used to treat obesity, with minimal side effects. Previous studies have reported that PA effectively improves body composition, chronic diseases, cardiovascular risk factors, and the quality of life [11,12,15]. To prevent obesity and chronic diseases, the World Health Organization (WHO) recommends performing aerobic exercise for at least 150 to 300 minutes weekly and muscle strength exercises more than twice a week [15]. Previous studies have reported that the participation of women in exercise is considerably less compared to that of men [16]. Therefore, an easy-to-access exercise intervention plan is needed to increase exercise participation.
Recently, research has been conducted to verify the effectiveness of various exercise intervention programs using mobile health (mHealth), including wearable devices (such as smartphones and smartwatches) and mobile apps [7,17,18]. Wearable devices are effective tools for PA and health management as they can easily monitor individual PA and health status [7,19]. Previous studies have shown that moderate-to-vigorous-intensity physical activity using mHealth reduces body weight [20]. In another study, blood pressure and lipid levels were improved by recording health status and monitoring physical activity using an mHealth app [21,22].
Therefore, this study aimed to verify the effect of a 12-week non-face-to-face exercise intervention using mHealth on body composition, health-related physical fitness, and blood lipid levels in obese women.
METHODS
Participants
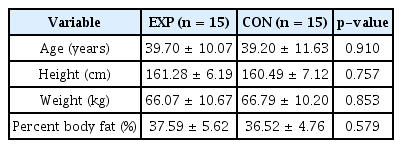
A total of 30 obese women (aged: 39.40 ± 11.07 years; percent body fat (%BF): 37.05 ± 5.15%) were enrolled, and all completed the study. This study was approved by the Institutional Review Board of Konkuk University( 7001355-202112-HR-491) and was conducted according to the principles of the Declaration of Helsinki. Written informed consent was obtained from all the participants, and their physical characteristics are listed in Table 1.
Non-face-to-face mHealth movement intervention
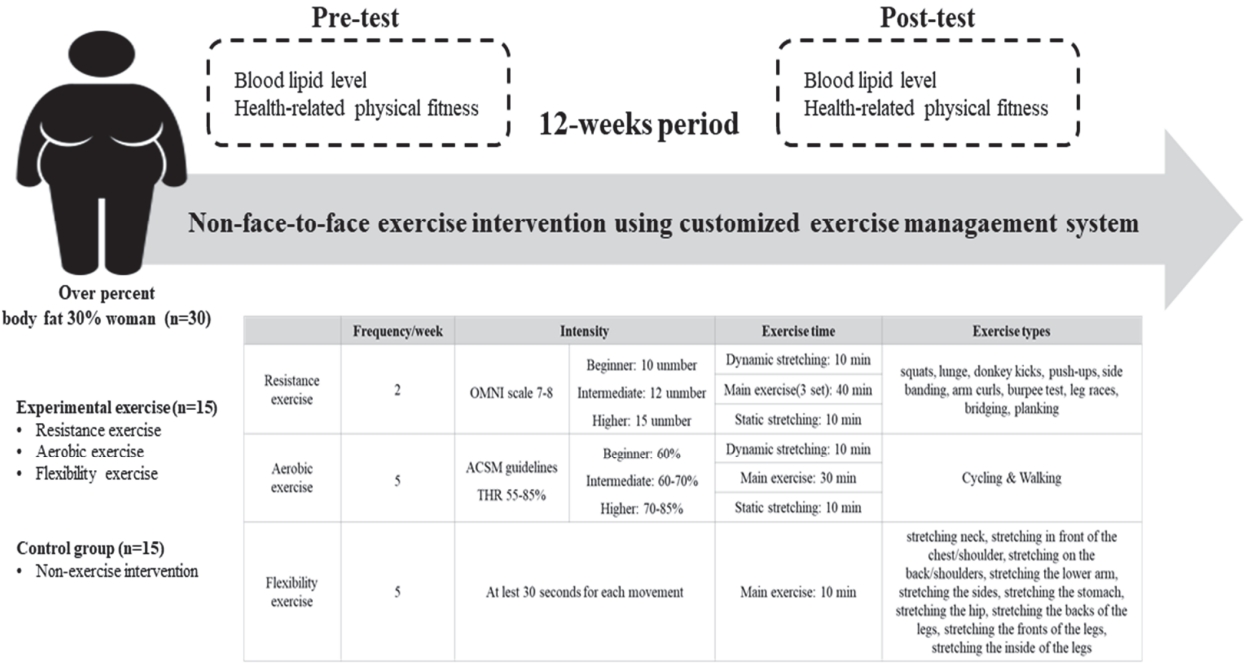
Non-face-to-face exercises were performed for 12 weeks using a mHealth and smart tracker (Charge 4, Fitbit, USA). The participants in this study were randomly assigned to the experimental (EXP) or control (CON) groups. The EXP group underwent non-face-to-face exercise intervention using mHealth, and the CON was recommended to maintain a routine during the intervention period. The exercise programs in the EXP included resistance (OMNI scale 7–8), aerobics (60–85% of the maximal heart rate [HRmax]), and flexibility (at least 30 s for each movement) [7]. The resistance exercise consisted of 10 movements and was performed twice a week for 60 min (including 10 min of warm-up, 40 min of the main exercise, and 10 min of cool-down). Resistance exercises included squats, lunges, donkey kicks, push-ups, side-banding, arm curls, burpee tests, leg races, bridging, and planking. Aerobic exercises were performed five times a week for 50 min (including 10 min of warmup, 30 min of the main exercise, and 10 min of cool-down). The aerobic exercises included cycling and walking. The flexibility exercise consisted of 11 movements and was performed five times a weekly for 10 min (at least 30 s for each movement). Flexibility exercises included stretching the neck, front of the chest/shoulder, back/shoulders, lower arm, sides, stomach, hip, backs of the legs, fronts of the legs, and insides of the legs. The study design for non-faceto-face exercise interventions using mHealth is shown in Figure 1.
Measurements
Body composition
Body composition was measured using an Inbody 770 (Inbody, Seoul, Korea) and BSM 330 (Inbody, Seoul, Korea). The participants maintained an empty stomach for 8 h before measurement and restricted PA for 48 h. Metallic substances attached to the body were removed before measurement and measurements were taken barefoot. Height, weight, and %BF were measured as test items.
Blood lipid levels
Blood lipid levels were measured using SD LipidoCare (SD Biosensor Inc., Seoul, Korea). Participants fasted for at least 8 h one day prior to the test, discarded the first drop of blood using the finger-tip method, and collected and measured 20 μL of blood23. TG, TC, HDL-C, and LDL-C were measured.
Health-related physical fitness
Health-related physical fitness tests included cardiorespiratory endurance (peak oxygen uptake [VO2peak]), muscular endurance (sit-ups), isometric muscle strength (grip strength), and flexibility (sit-and-reach).
Cardiopulmonary endurance was measured as VO2peak (mL·kg·min−1) using a cycle ergometer (Aerobike 75XLII, Konami, Tokyo, Japan). The saddle height was adjusted according to the participants sitting on the cycle ergometer. Age and sex were recorded, a heart rate detection sensor was attached to the earlobe, and measurements were initiated when the heart rate showed a stable level. The pedal was applied at a speed of 50 rpm, and the bicycle load was gradually increased in response to the subject’s heart rate information, which was terminated when the heart rate reached 75% of HRmax. A target heart rate of 75% HRmax was calculated and set using the predicted HRmax formula (male: 209–0.69 × age, female: 205–0.75 × age).
Muscle endurance was measured during sit-ups. When the participant went down for 60 s, the scapula was completely in contact with the floor, and the number of times both elbows accurately touched the knee when rising was recorded; if it was not performed with accurate movements, it was excluded from the record.
Isometric muscle strength was measured using a grip meter (T.K.K.5001, TAKEI, Tokyo, Japan). After adjusting the grip strength meter handle to fit the second joint of the participant’s finger, the participants measured both arms twice with the measuring arm 45° away from the body and recorded a good score in units of 0.1 kg.
Flexibility was measured by sitting with a left-buckling measuring instrument (T.K.K. 5403, Flexion-D, Tokyo, Japan). The participants removed their socks, placed the sole on the vertical surface of the measuring instrument barefoot, and slowly bent the upper body according to the start signal so that the middle fingers of both hands touched the measuring instrument simultaneously. If the correct posture was not maintained, it was judged to be invalid, and after a total of two measurements, the maximum value was recorded in units of 0.1 cm.
Statistical analysis
This was verified using G*Power 3.1.9.2 (Franz Faul, University of Kiel, Kiel, Germany) to improve the power to 95% or higher. All statistical tests were performed with an effect size of 0.57, a significance level of 0.05 (α = 0.05), and a power of 0.85. G*Power showed that 10 participants had sufficient power for this study (Gell et al., 2020). However, 30 participants were selected considering the number of dropouts during the 12-week exercise intervention. The mean and standard deviation values were calculated using SPSS 28 (IBM Corp., Armonk, NY, USA) for statistical analysis. The normality of all dependent variable distributions was verified using the Shapiro-Wilk test. A two-way repeated-measures ANOVA was conducted to verify the interaction effect between the group and intervention period. A paired t-test was conducted to determine changes within the group according to training. The significance level for all statistical analyses was set at p < 0.05.
RESULTS
Energy expenditure
Figure 2 shows changes in exercise energy expenditure (EEE) and total energy expenditure (TEE) during the nonface- to-face exercise intervention period. The main effects between groups are shown in EEE, and significant interactions and main effects between groups are shown in TEE. As a result of the post-hoc analysis, the TEE (Post − Pre 1: 364.17 kcal·day−1, p<0.001) in the EXP increased significantly. There was a significant difference in pre-(EXP − CON:119.9 kcal, p < 0.01), middle-(EXP − CON:158.24 kcal, p < 0.001), and post-(EXP − CON: 181.54 kcal, p < 0.001) intervention tests between the two groups.
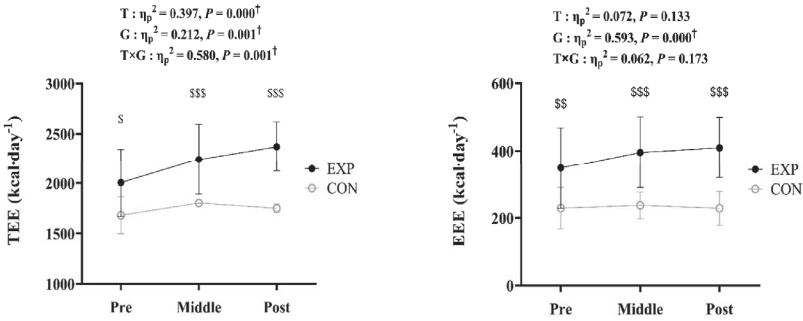
Changes in energy expenditure among the pre-, middle-, and post-intervention tests. EXP: experimental group, CON: control group. TEE: total energy expenditure, EEE: exercise energy expenditure. ✝p < 0.05, significant interaction or main effect. $p < 0.05, $$p < 0.01, $$$p < 0.001 significant difference between the groups.
Blood lipid levels
Figure 3 shows the changes in blood lipid levels during the non-face-to-face exercise intervention period using mHealth. Significant interactions and main effects were observed for HDL-C, and inter-period main effects were observed for the LDL-C/HDL-C ratio. The post-hoc analysis showed a significant increase in HDL-C (Post − Pre:9.07 mg·dL−1, p < 0.001) in EXP and a significant decrease in LDL-C/HDL-C ratio (Post − Pre: −0.71 mg·dL−1, p < 0.05).
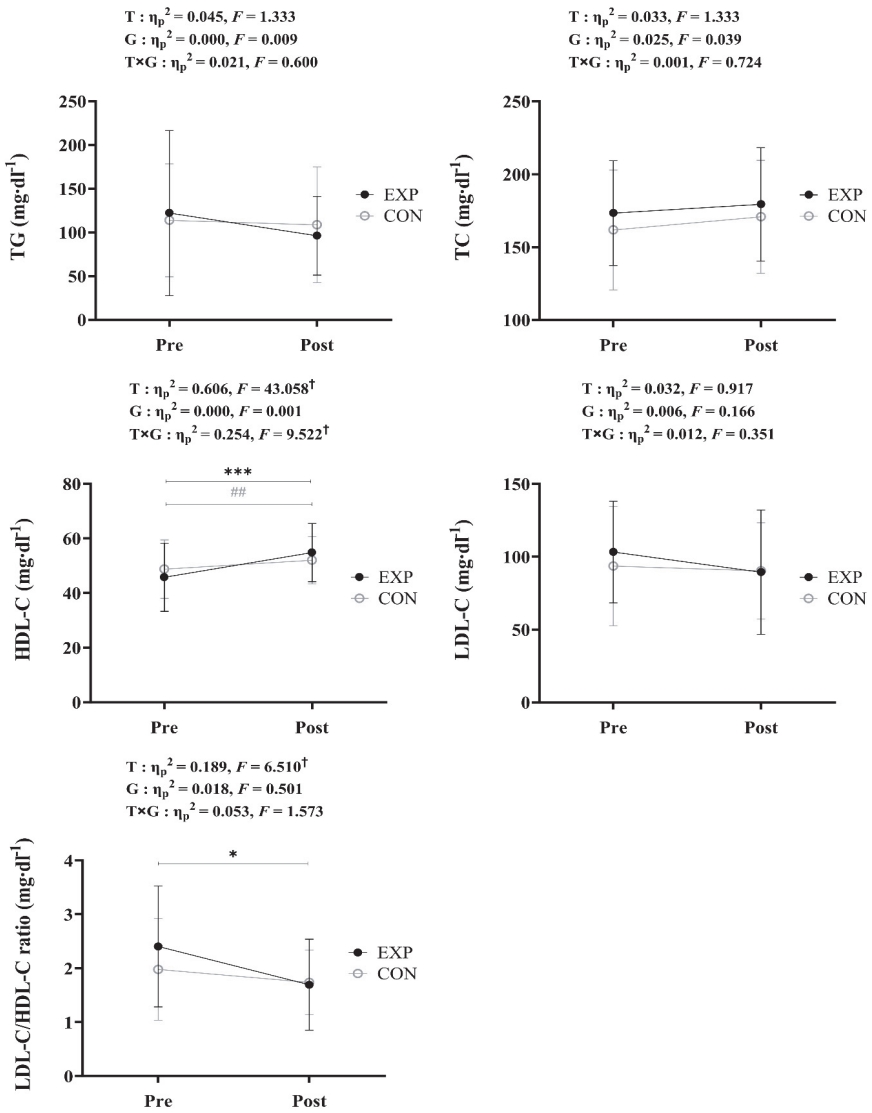
Changes in blood lipid levels between the pre- and post-intervention tests. EXP: experimental group, CON: control group. TG: total cholesterol, TC: triglyceride, HDL-C: high-density lipoprotein cholesterol, LDL-C: low-density lipoprotein cholesterol. ✝p < 0.05, significant interaction or main effect. *p < 0.05, ***p < 0.001, significant difference between the pre- and post- intervention tests in EXP group. ##p < 0.01, significant difference between the pre- and post- intervention tests in CON group.
Health-related physical fitness
Figure 4 shows the changes in health-related physical fitness during the non-face-to-face exercise intervention period using mHealth. Significant interaction and main effects were shown in sit-ups, and intervention period main effects were shown in grip strength and sit-and-reach. Post-hoc analysis showed a significant increase in sit-ups (Post − Pre: 7.73, p < 0.001) in the EXP and in grip strength (Post − Pre: 2.92 kg, p < 0.001) and sit and reach (Post − Pre: 2.51 cm, p < 0.01) between intervention periods.
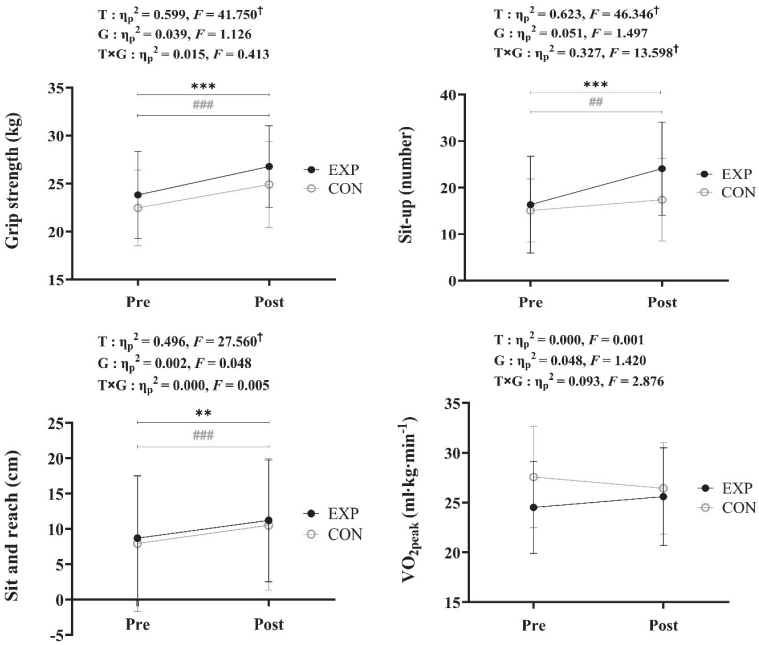
Changes in health-related physical fitness between the pre- and post-intervention tests. EXP: experimental group, CON: control group. ✝p<0.05, significant interaction or main effect. **p < 0.01, ***p < 0.001, significant difference between the pre- and post- intervention tests in EXP group. ##p < 0.01, ###p < 0.001, significant difference between the pre- and post- intervention tests in CON group.
DISCUSSION
This study was designed assuming that 12 weeks of a nonface- to-face exercise intervention using mHealth would improve blood lipid levels and health-related physical fitness in obese women. As a result, non-face-to-face exercise intervention using mHealth decreased the LDL-C/HDL-C ratio and increased grip strength, sit-ups, sit-and-reach, and HDL-C.
Appropriate exercise can prevent obesity and chronic diseases [15]. With technological advancement, various exercise programs using wearable and mHealth devices are being developed and many studies are being conducted to treat and prevent obesity [7,17,24,25]. Kusnanto et al. [22] reported that 12 weeks of physical activity and programs using an app improved the TC, TG, and LDL-C levels in patients with type 2 diabetes. In addition, it was reported that this application could demonstrate the benefits of physical activity by allowing independent management through easy access, which improved telecommunication difficulties. Hamaya et al. [26] reported that PA using mHealth improved LDL-C levels, based on data from 5473 people registered on the Kencom app in Japan. In this study, non-face-to-face complex exercises (resistance, aerobic, and flexibility) were conducted using a wearable device and mHealth to improve the various risks of obesity. Positive results were obtained to improve blood lipid levels. Some researchers have reported that high-intensity aerobic exercise can significantly improve blood lipid levels [27,28], whereas other researchers have reported that moderate-intensity aerobic exercise can significantly improve blood lipid levels [28-30]). Oh et al. [28] reported that moderate- and vigorous-intensity aerobic exercises and combined exercise (aerobic and resistance) improved blood lipid levels. In this study’s non-face-to-face complex exercise program, exercise intensity (medium to high intensity) was determined according to the participants’ goal setting and physical fitness level. From this perspective, the exercise intensity in this study was appropriately set according to the results of previous studies, resulting in positive results for the blood lipid levels of obese women. However, blood lipid levels can be considerably influenced by diet [31]. In future studies, it is believed that a combination of exercise and dietary intervention will have a more positive effect on blood lipid level improvement than exercise intervention alone.
Health-related physical fitness refers to the ability to perform activities of daily living with vitality [32]. Health-related physical fitness is closely related to disease and mortality; therefore, improving physical fitness through PA is important [33,34]. Stork et al. [35] reported positive changes in flexibility and muscular endurance after 8 weeks of exercise intervention using the mHealth app. Avila et al. [36] reported that grip strength, flexibility, and VO2peak tended to increase after 150 min of home training per week for 12 weeks in 90 patients with coronary artery disease. However, another study reported no change in physical strength when PA was administered using a Wii Fit in eight households [37]. Owens et al. [37] reported that there was no change in physical fitness because of the lack of physiological stimulation owing to the low intensity of PA intervention using Wii Fit. This study performed moderate-intensity aerobic exercise for at least 150 min per week and moderate-intensity strength exercise at least twice per week according to the ACSM. Positive results have been obtained for improving health-related physical fitness through wearable devices and mHealth. Therefore, a non-face-to-face exercise intervention program can positively affect health-related physical fitness if appropriate exercise prescriptions and monitoring are provided.
This study observed that non-face-to-face exercise using mHealth for 12 weeks improved blood lipid levels and health-related physical fitness. Wearable devices and mHealth can set exercise goals, provide customized feedback without expert prescriptions, and improve compliance through self-monitoring to improve lifestyle through increased PA.
Because this study was a non-face-to-face exercise intervention through mHealth, there were limitations in providing complete control and accurate coaching of exercise posture. In addition, there were no co-interventions for dietary management. Better research results will likely be obtained if various technologies such as mHealth and motion recognition are developed in the future and intervened along with dietary management.
Acknowledgements
The authors have no financial, consulting, institutional, or other relationships that may lead to bias or conflicts of interest.