1. Meyer SA, Kulkarni AP. Hepatotoxicity. et al, Hodgson E, (ed) Smart RCIntroduction to biochemical toxicology. 3rd ed. New York: John Wiley & Sons. p. 487-90. 2001.
2. Uličná O, Greksák M, Vančová O, Zlatoš L, Galbavỳ Ŝ, Božek P, Nakano M. Hepatoprotective effect of rooibos tea (Aspalathus linearis) on CCl4-induced liver damage in rats.
Physiol Res 2003;52:461-6. PMID:
12899659.
3. Ponnappa BC, Rubin E. Modeling alcohol’s effects on organs in animal models.
Alcohol Res Health 2000;24:93-104. PMID:
11199283.
4. Song Z, Deaciuc I, Song M, Lee DY, Liu Y, Ji X, McClain C. Silymarin protects against acute ethanol-induced hepatotoxicity in mice.
Alcohol Clin Exp Res 2006;30:407-13. PMID:
10.1111/j.1530-0277.2006.00063.x. PMID:
16499481.

5. Yang P, Wang Z, Zhan Y, Wang T, Zhou M, Xia L, Yang X, Zhang J. Endogenous A1 adenosine receptor protects mice from acute ethanol-induced hepatotoxicity.
Toxicology 2013;309:100-6. PMID:
10.1016/j.tox.2013.05.003. PMID:
23692951.

6. Rao RK, Seth A, Sheth P. Recent Advances in Alcoholic Liver Disease I. Role of intestinal permeability and endotoxemia in alcoholic liver disease.
Am J Physiol Gastrointest Liver Physiol 2004;286:G881-4. PMID:
10.1152/ajpgi.00006.2004. PMID:
15132946.

7. Xing WW, Zou MJ, Liu S, Xu T, Wang JX, Xu DG. Interleukin-22 protects against acute alcohol-induced hepatotoxicity in mice.
Biosci Biotechnol Biochem 2011;75:1290-4. PMID:
10.1271/bbb.110061. PMID:
21737938.

8. Nordmann R. Alcohol and antioxidant systems.
Alcohol Alcohol 1994;29:513-22. PMID:
7811335.
9. Kurose I, Higuchi H, Kato S, Miura S, Watanabe N, Kamegaya Y, Tomita K, Takaishi M, Horie Y, Fukuda M, Mizukami K, Ishii H. Oxidative stress on mitochondria and cell membrane of cultured rat hepatocytes and perfused liver exposed to ethanol.
Gastroenterology 1997;112:1331-43. PMID:
10.1016/S0016-5085(97)70147-1. PMID:
9098019.

10. Rouach H, Fataccioli V, Gentil M, French SW, Morimoto M, Nordmann R. Effect of chronic ethanol feeding on lipid peroxidation and protein oxidation in relation to liver pathology.
Hepatology 1997;25:351-5. PMID:
10.1002/hep.510250216. PMID:
9021946.

11. Bondy SC, Orozco J. Effects of ethanol treatment upon sources of reactive oxygen species in brain and liver.
Alcohol Alcohol 1994;29:375-83. PMID:
7986274.
13. Somani SM. Exercise, drugs and tissue specific antioxidant system. et al, (Ed.) Somani SMPharmacology in Exercise and Sports. Boca Raton: FL: CRC Press. p. 57-95. 1996.
15. Wang T, Yang P, Zhan Y, Xia L, Hua Z, Zhang J. Deletion of circadian gene Per1 alleviates acute ethanol-induced hepatotoxicity in mice.
Toxicology 2013;314:193-201. PMID:
10.1016/j.tox.2013.09.009. PMID:
24144995.

16. Lu Y, Zhuge J, Wang X, Bai J. Cederbaum AI. Cytochrome P450 2E1 contributes to ethanol-induced fatty liver in mice.
Hepatology 2008;47:1483-94. PMID:
18393316.

17. Kobayashi M, Yamamoto M. Molecular mechanisms activating the Nrf2-Keap1 pathway of antioxidant gene regulation. Antioxid.
Redox Signal 2005;7:385-94. PMID:
10.1089/ars.2005.7.385.

19. Lee JM, Li J, Johnson DA, Stein TD, Kraft AD, Calkins MJ, Jakel RJ, Johnson JA. Nrf2, a multi-organ protector?
FASEB J 2005;19:1061-6. PMID:
10.1096/fj.04-2591hyp. PMID:
15985529.

21. Zeng T, Xie KQ. Ethanol and liver: recent advances in the mechanisms of ethanol-induced hepatosteatosis.
Arch Toxicol 2009;83:1075-81. PMID:
10.1007/s00204-009-0457-4. PMID:
19588123.


22. Herzig S, Hedrick S, Morantte I, Koo SH, Galimi F, Montminy M. CREB controls hepatic lipid metabolism through nuclear hormone receptor PPAR-gamma.
Nature 2003;426:190-3. PMID:
10.1038/nature02110. PMID:
14614508.


23. Wada S, Yamazaki T, Kawano Y, Miura S, Ezaki O. Fish oil fed prior toethanol administration prevents acute ethanol-induced fatty liver in mice.
J Hepatol 2008;49:441-50. PMID:
10.1016/j.jhep.2008.04.026. PMID:
18620774.

24. Yu S, Matsusue K, Kashireddy P, Cao WQ, Yeldandi V, Yeldandi AV, Rao MS, Gonzalez FJ, Reddy JK. Adipocyte-specific gene expressionand adipogenic steatosis in the mouse liver due to peroxisome proliferator-activated receptor gamma1 (PPARgamma1) overexpression.
J Biol Chem 2003;278:498-505. PMID:
10.1074/jbc.M210062200. PMID:
12401792.

26. Devipriya N, Srinivasan M, Sudheer AR, Menon VP. Effect of ellagic acid, a natural polyphenol, on alcohol-induced prooxidant and antioxidant imbalance: a drug dose dependent study.
Singapore Med J 2007;48:311-8. PMID:
17384878.
27. Jafri MA, Jalis Subhani M, Javed K, Singh S. Hepatoprotective activity of leaves of Cassia occidentalis against paracetamol and ethyl alcohol intoxication in rats.
J Ethnopharmacol 1999;66:355-61. PMID:
10.1016/S0378-8741(99)00037-9. PMID:
10473185.

28. Kaviarasan S, Anuradha CV. Fenugreek (Trigonella foenum graecum) seed polyphenols protect liver from alcohol toxicity: a role on hepatic detoxification system and apoptosis.
Pharmazie 2007;62:299-304. PMID:
17484288.
29. Kumar RS, Ponmozhi M, Viswanathan P, Nalini N. Effect of Cassia auriculata leaf extract on lipids in rats with alcoholic liver injury.
Asia Pac J Clin Nutr 2002;11:157-63. PMID:
10.1046/j.1440-6047.2002.00286.x. PMID:
12074184.

30. Saravanan R, Viswanathan P, Pugalendi KV. Protective effect of ursolic acid on ethanol-mediated experimental liver damage in rats.
Life Sci 2006;78:713-8. PMID:
10.1016/j.lfs.2005.05.060. PMID:
16137716.

31. Kim HL, Sim JE, Choi HM, Choi IY, Jeong MY, Park J, Jung Y, Youn DH, Cho JH, Kim JH, Hwang MW, Jin JS, Hong SH, Cho HW, Um JY. The AMPK pathway mediates an anti-adipogenic effect of fruits of Hovenia dulcis Thunb.
Food Funct 2014;5:2961-8. PMID:
10.1039/C4FO00470A. PMID:
25224378.

32. Na CS, Yoon SY, Kim JB, Na DS, Dong MS, Lee MY, Hong CY. Anti-fatigue activity of Hovenia dulcis on a swimming mouse model through the inhibition of stress hormone expression and antioxidation.
J Chin Med 2013;41:945-55. PMID:
10.1142/S0192415X13500638.

33. Li G, Min BS, Zheng C, Lee J, Oh SR, Ahn KS, Lee HK. Neuroprotective and free radical scavenging activities of phenolic compounds from Hovenia dulcis.
Arch Pharm Res 2005;28:804-9. PMID:
10.1007/BF02977346. PMID:
16114495.


34. Hase K, Ohsugi M, Xiong Q, Basnet P, Kadota S, Namba T. Hepatoprotective effect of Hovenia dulcis THUNB. on experimental liver injuries induced by carbon tetrachloride or D-galactosamine/ lipopolysaccharide.
Biol Pharm Bull 1997;20:381-5. PMID:
10.1248/bpb.20.381. PMID:
9145214.

35. Wang M, Zhu P, Jiang C, Ma L, Zhang Z, Zeng X. Preliminary characterization, antioxidant activity in vitro and hepatoprotective effect on acute alcohol-induced liver injury in mice of polysaccharides from the peduncles of Hovenia dulcis.
Food Chem Toxicol 2012;50:2964-70. PMID:
10.1016/j.fct.2012.06.034. PMID:
22750723.

36. Butler WM, Maling HM, Horning MG, Brodie BB. The direct determination of liver triglycerides. J Lipid Res. 1961;2:95-6. Bondy SC, Orozco J. Effects of ethanol treatment upon sources of reactive oxygen species in brain and liver.
Alcohol Alcohol 1994;29:375-83. PMID:
7986274.
37. Bucolo G, David H. Quantitative determination of serum triglycerides by the use of enzymes.
Clin Chem 1973;19:476-82. PMID:
4703655.


38. Lowry OH, Rosenbrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent.
J Biol Chem 1951;193:265-75. PMID:
14907713.

39. Hotchkiss RS, Osborne DF, Lappas GD, Karl IE. Calcium antagonists decrease plasma and tissue concentrations of tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-1 alpha in a mouse model of endotoxin.
Shock 1995;3:337-42. PMID:
7648334.
40. Yoon HS, Kim JW, Cho HR, Moon SB, Shin HD, Yang KJ, Lee HS, Kwon YS, Ku SK. Immunomodulatory effects of Aureobasidium pullulans SM-2001 exopolymers on the cyclophosphamide-treated mice.
J Microbiol Biotechnol 2010;20:438-45. PMID:
20208453.

41. Clark BD, Bedrosian I, Schindler R, Cominelli F, Cannon JG, Shaw AR, Dinarello CA. Detection of interleukin 1 alpha and 1 beta in rabbit tissues during endotoxemia using sensitive radioimmunoassays.
J Appl Physiol (1985) 1991;71:2412-8. PMID:
1778940.

42. Kavutcu M, Canbolat O, Oztürk S, Olcay E, Ulutepe S, Ekinci C, Gökhun IH, Durak I. Reduced enzymatic antioxidant defense mechanism in kidney tissues from gentamicin-treated guinea pigs: effects of vitamins E and C.
Nephron 1996;72:269-74. PMID:
10.1159/000188853. PMID:
8684538.

43. Jamall IS, Smith JC. Effects of cadmium on glutathione peroxidase superoxidase dismutase and lipid peroxidation in the rat heart: a possible mechanism of cadmium cardiotoxicity.
Toxicol Appl Pharmacol 1985;80:33-42. PMID:
10.1016/0041-008X(85)90098-5. PMID:
4024106.

44. Sedlak J, Lindsay RH. Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent.
Anal Biochem 1968;25:192-205. PMID:
10.1016/0003-2697(68)90092-4. PMID:
4973948.

45. Aebi H. Catalase. (Ed.) Bergmeyer HUMethods in Enzymatic Analysis. New York: Academic Press. p. 673-86. 1974.
46. Sun Y, Larry WO, Ying L. A simple method for clinical assay of superoxide dismutase.
Clin Chem 1988;34:497-500. PMID:
3349599.


47. Jung YM, Lee SH, Lee DS, You MJ, Chung IK, Cheon WH, Kwon YS, Lee YJ, Ku SK. Fermented garlic protects diabetic, obese mice when fed a high-fat diet by antioxidant effects.
Nutr Res 2011;31:387-96. PMID:
10.1016/j.nutres.2011.04.005. PMID:
21636017.

48. Ki SH, Yang JH, Ku SK, Kim SC, Kim YW, Cho IJ. Red ginseng extract protects against carbon tetrachloride-induced liver fibrosis.
J Ginseng Res 2013;37:45-53. PMID:
10.5142/jgr.2013.37.45. PMID:
23717156.

49. Shi SR, Chaiwun B, Young L, Cote RJ, Taylor CR. Antigen retrieval technique utilizing citrate buffer or urea solution for immunohistochemical demonstration of androgen receptor in formalin-fixed paraffin sections.
J Histochem Cytochem 1993;41:1599-604. PMID:
10.1177/41.11.7691930. PMID:
7691930.

50. Li SY, Yang D, Fu ZJ, Woo T, Wong D, Lo AC. Lutein enhances survival and reduces neuronal damage in a mouse model of ischemic stroke.
Neurobiol Dis 2012;45:624-32. PMID:
10.1016/j.nbd.2011.10.008. PMID:
22024715.

51. Chen JH, Tipoe GL, Liong EC, So HS, Leung KM, Tom WM, Fung PC, Nanji AA. Green tea polyphenols prevent toxin-induced hepatotoxicity in mice by down-regulating inducible nitric oxide-derived prooxidants.
Am J Clin Nutr 2004;80:742-51. PMID:
15321817.


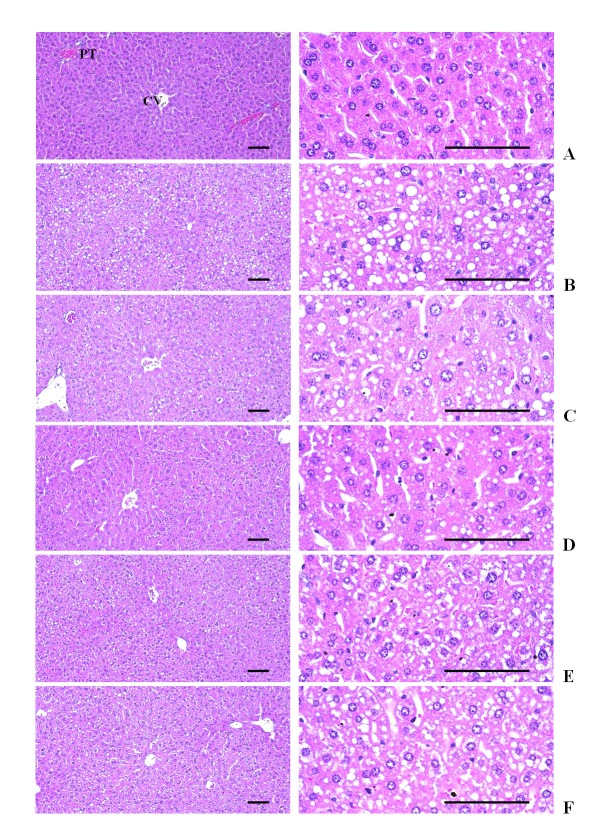
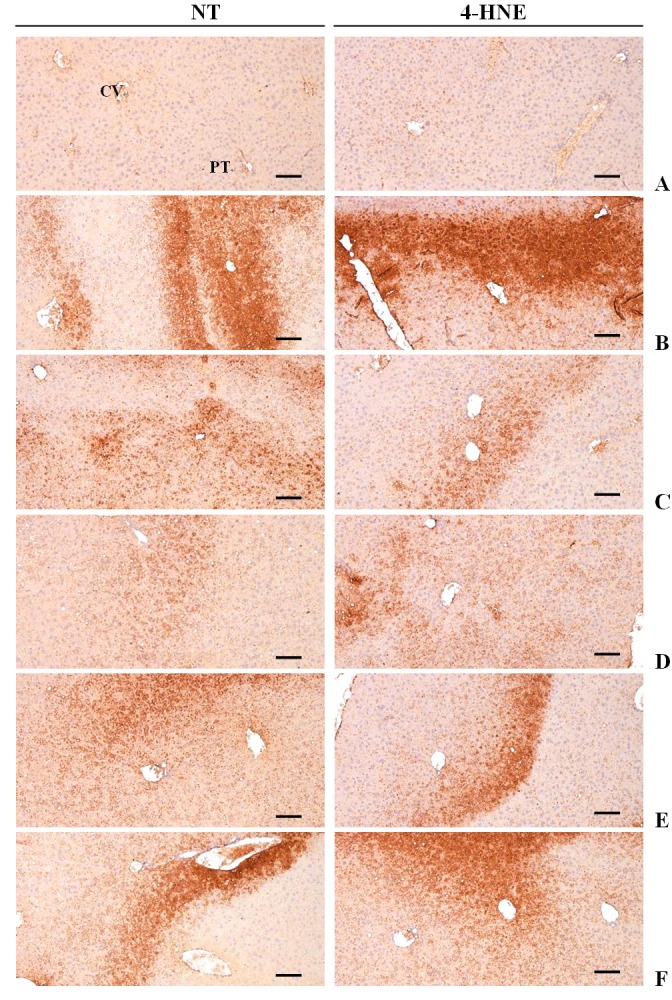
52. Hartley DP, Kolaja KL, Reichard J, Petersen DR. 4-Hydroxynonenal and malondialdehyde hepatic protein adducts in rats treated with carbon tetrachloride: immunochemical detection and lobular localization.
Toxicol Appl Pharmacol 1999;161:23-33. PMID:
10.1006/taap.1999.8788. PMID:
10558920.

53. Noyan S, Cavusoglu I, Minbay FZ. The effect of vitamin A on EtOH-induced hepatic injuries in rats: a histochemical, immunohistochemical and ultrastructural study.
Acta Histochem 2006;107:421-34. PMID:
16256175.

56. Kang SJ, Lee JE, Lee EK, Jung DH, Song CH, Park SJ, Choi SH, Han CH, Ku SK, Lee YJ. Fermentation with Aquilariae Lignum enhances the anti-diabetic activity of green tea in type II diabetic db/db mouse.
Nutrients 2014;6:3536-71. PMID:
10.3390/nu6093536. PMID:
25207824.

58. Smathers RL, Galligan JJ, Stewart BJ, Petersen DR. Overview of lipid peroxidation products and hepatic protein modification in alcoholic liver disease.
Chem Biol Interact 2011;192:107-12. PMID:
10.1016/j.cbi.2011.02.021. PMID:
21354120.

60. Hu M, Yin H, Mitra MS, Liang X, Ajmo JM, Nadra K, Chrast R, Finck BN, You M. Hepatic-specific lipin-1 deficiency exacerbates experimental alcohol-induced steatohepatitis in mice.
Hepatology 2013;58:1953-63. PMID:
10.1002/hep.26589. PMID:
23787969.

61. Saravanan N, Nalini N. Inhibitory effect of Hemidesmus indicus and its active principle 2-hydroxy 4-methoxy benzoic acid on ethanol-induced liver injury.
Fundam Clin Pharmacol 2007;21:507-14. PMID:
10.1111/j.1472-8206.2007.00500.x. PMID:
17868203.

62. Saravanan N, Rajasankar S, Nalini N. Antioxidant effect of 2-hydroxy-4-methoxy benzoic acid on ethanol-induced hepatotoxicity in rats.
J Pharm Pharmacol 2007;59:445-53. PMID:
10.1211/jpp.59.3.0015. PMID:
17331349.

63. Gopumadhavan S, Rafiq M, Azeemuddin M, Mitra SK. Ameliorative effect of Partysmart in rat model of alcoholic liver disease.
Indian J Exp Biol 2008;46:132-7. PMID:
18335812.
64. Kasdallah-Grissa A, Mornagui B, Aouani E, Hammami M, El May M, Gharbi N, Kamoun A, El-Fazaâ S. Resveratrol, a red wine polyphenol, attenuates ethanol-induced oxidative stress in rat liver.
Life Sci 2007;80:1033-9. PMID:
10.1016/j.lfs.2006.11.044. PMID:
17258234.

65. Pari L, Suresh A. Effect of grape (Vitis vinifera L.) leaf extract on alcohol induced oxidative stress in rats.
Food Chem Toxicol 2008;46:1627-34. PMID:
10.1016/j.fct.2008.01.003. PMID:
18289759.

66. Zhang R, Hu Y, Yuan J, Wu D. Effects of Puerariae radix extract on the increasing intestinal permeability in rat with alcohol-induced liver injury.
J Ethnopharmacol 2009;126:207-14. PMID:
10.1016/j.jep.2009.08.044. PMID:
19735712.

67. Park JH, Kim SJ, Hwang I, Bae KC, Bae JH, Song DK. Green tea extract co-administered with a polymer effectively prevents alcoholic liver damage by prolonged inhibition of alcohol absorption in mice.
Alcohol Alcohol 2013;48:59-67. PMID:
10.1093/alcalc/ags118. PMID:
23136046.


68. Sodikoff CH. Laboratory profiles of small animal diseases, A guide to laboratory diagnosis. St. Louise: Mosby 1995;1-36.
69. Das SK, Varadhan S, Gupta G, Mukherjee S, Dhanya L, Rao DN, Vasudevan DM. Time-dependent effects of ethanol on blood oxidative stress parameters and cytokines.
Indian J Biochem Biophys 2009;46:116-21. PMID:
19374264.
70. Li YM, Chen SH, Yu CH, Zhang Y, Xu GY. Effect of acute alcoholism on hepatic enzymes and oxidation/antioxidation in rats.
Hepatobiliary Pancreat Dis Int 2004;3:241-4. PMID:
15138118.
71. Ho WY, Yeap SK, Ho CL, Abdul Rahim R, Alitheen NB. Hepatoprotective activity of Elephantopus scaber on alcohol-induced liver damage in mice.
Evid Based Complement Alternat Med 2012;2012:417953PMID:
22973401.


72. Xiang J, Zhu W, Li Z, Ling S. Effect of juice and fermented vinegar from Hovenia dulcis peduncles on chronically alcohol-induced liver damage in mice.
Food Funct 2012;3:628-34. PMID:
10.1039/c2fo10266h. PMID:
22648047.

73. McClain CJ, Cohen DA. Increased tumor necrosis factor production by monocytes in alcoholic hepatitis.
Hepatology 1989;9:349-51. PMID:
10.1002/hep.1840090302. PMID:
2920991.

74. Iimuro Y, Gallucci RM, Luster MI, Kono H, Thurman RG. Antibodies to tumor necrosis factor alfa attenuate hepatic necrosis and inflammation caused by chronic exposure to ethanol in the rat.
Hepatology 1997;12;26(6):1530-7. PMID:
10.1002/hep.510260621. PMID:
9397994.

75. Yin M, Wheeler MD, Kono H, Bradford BU, Gallucci RM, Luster MI, Thurman RG. Essential role of tumor necrosis factor alpha in alcohol-induced liver injury in mice.
Gastroenterology 1999;117:942-52. PMID:
10.1016/S0016-5085(99)70354-9. PMID:
10500078.

76. Zhou Z, Sun X, James Kang Y. Metallothionein protection against alcoholic liver injury through inhibition of oxidative stress.
Exp Biol Med 2002;227:214-22.

77. Dehmlow C, Erhard J, Groot H. Inhibition of Kupffer cell functions as an explanation for the hepatoprotective properties of silibinin.
Hepatology 1996;23:749-54. PMID:
10.1002/hep.510230415. PMID:
8666328.

78. Cho JY, Kim PS, Park J, Yoo ES, Baik KU, Kim YK, Park MH. Inhibitor of tumor necrosis factor-alpha production in lipopolysaccharide- stimulated RAW264.7 cells from Amorpha fruticosa.
J Ethnopharmacol 2000;70:127-33. PMID:
10.1016/S0378-8741(99)00154-3. PMID:
10771202.

79. Lieber C. Cytochrome P-4502E1: its physiological and pathological role.
Physiol Rev 1997;77:517-44. PMID:
9114822.

80. Gouillon Z, Lucas D, Li J, Hagbjork AL, French BA, Fu P, Fang C, Ingelman-Sundberg M, Donohue TM Jr., French SW. Inhibition of ethanol-induced liver disease in the intragastric feeding rat model by chlormethiazole.
Proc Soc Exp Biol Med 2000;224:302-9. PMID:
10964266.

81. McCarty MF. Inhibition of CYP2E1 with natural agents may be a feasible strategy for minimizing the hepatotoxicity of ethanol.
Med Hypotheses 2001;56:8-11. PMID:
10.1054/mehy.1999.1015. PMID:
11133247.

82. Morgan K, French SW, Morgan TR. Production of a cytochrome P450 2E1 transgenic mouse and initial evaluation of alcoholic liver damage.
Hepatology 2002;36:122-34. PMID:
10.1053/jhep.2002.33720. PMID:
12085356.

83. Cahill A, Cunningham CC, Adachi M, Ishii H, Bailey SM, Fromenty B, Davies A. Effects of alcohol and oxidative stress on liver pathology: the role of the mitochondrion.
Alcohol Clin Exp Res 2002;26:907-15. PMID:
10.1111/j.1530-0277.2002.tb02621.x. PMID:
12068261.

84. Castilla R, González R, Fouad D, Fraga E, Muntané J. Dual effect of ethanol on cell death in primary culture of human and rat hepatocytes.
Alcohol Alcohol 2004;39:290-6. PMID:
10.1093/alcalc/agh065. PMID:
15208159.


85. Navasumrit P, Ward TH, Dodd NJ, O’Connor PJ. Ethanol-induced free radicals and hepatic DNA strand breaks are prevented in vivo by antioxidants: effects of acute and chronic ethanol exposure.
Carcinogenesis 2000;21:93-9. PMID:
10.1093/carcin/21.1.93. PMID:
10607739.


86. Ozaras R, Tahan V, Aydin S, Uzun H, Kaya S, Senturk H. N-acetylcysteine attenuates alcohol-induced oxidative stress in the rat.
World J Gastroenterol 2003;9:125-8. PMID:
12508366.

87. Husain K, Scott BR, Reddy SK, Somani SM. Chronic ethanol and nicotine interaction on rat tissue antioxidant defense system.
Alcohol 2001;25:89-97. PMID:
10.1016/S0741-8329(01)00176-8. PMID:
11747978.

88. Koch O, Farré S, De Leo ME, Palozza P, Palazzotti B, Borrelo S, Palombini G, Cravero A, Galeotti T. Regulation of manganese superoxide dismutase (MnSOD) in chronic experimental alcoholism: effects of vitamin E-supplemented and -deficient diets.
Alcohol Alcohol 2000;35:159-63. PMID:
10.1093/alcalc/35.2.159. PMID:
10787391.


89. Subudhi U, Das K, Paital B, Bhanja S, Chainy GB. Alleviation of enhanced oxidative stress and oxygen consumption of L-thyroxine induced hyperthyroid rat liver mitochondria by vitamin E and curcumin.
Chem Biol Interact 2008;173:105-14. PMID:
10.1016/j.cbi.2008.02.005. PMID:
18377885.

90. Videla LA. Energy metabolism, thyroid calorigenesis, and oxidative stress: functional and cytotoxic consequences.
Redox Rep 2000;5:265-75. PMID:
10.1179/135100000101535807. PMID:
11145101.

91. Messarah M, Boumendjel A, Chouabia A, Klibet F, Abdennour C, Boulakoud MS, Feki AE. Influence of thyroid dysfunction on liver lipid peroxidation and antioxidant status in experimental rats.
Exp Toxicol Pathol 2010;62:301-10. PMID:
10.1016/j.etp.2009.04.009. PMID:
19540741.

93. Das K, Chainy GB. Modulation of rat liver mitochondrial antioxidant defence system by thyroid hormone.
Biochim Biophys Acta 2001;1537:1-13. PMID:
10.1016/S0925-4439(01)00048-5. PMID:
11476958.

94. Voldstedlund M, Tranum-Jensen J, Handberg A, Vinten J. Quantity of Na/K-ATPase and glucose transporters in the plasma membrane of rat adipocytes is reduced by in vivo triiodothyronine.
Eur J Endocrinol 1995;133:626-34. PMID:
10.1530/eje.0.1330626. PMID:
7581995.

95. Odabasoglu F, Cakir A, Suleyman H, Aslan A, Bayir Y, Halici M, Kazaz C. Gastroprotective and antioxidant effects of usnic acid on indomethacin-induced gastric ulcer in rats.
J Ethnopharmacol 2006;103:59-65. PMID:
10.1016/j.jep.2005.06.043. PMID:
16169175.

96. Cheeseman KH, Slater TF. An introduction to free radical biochemistry.
Br Med Bull 1993;49:481-93. PMID:
8221017.


97. Ji C, Chan C, Kaplowitz N. Predominant role of sterol response element binding proteins (SREBP) lipogenic pathways in hepatic steatosis in the murine intragastric ethanol feeding model.
J Hepatol 2006;45:717-24. PMID:
10.1016/j.jhep.2006.05.009. PMID:
16879892.

98. Crabb DW, Galli A, Fischer M, You M. Molecular mechanisms of alcoholic fatty liver: role of peroxisome proliferator-activated receptor alpha.
Alcohol 2004;34:35-8. PMID:
10.1016/j.alcohol.2004.07.005. PMID:
15670663.

99. Fischer M, You M, Matsumoto M, Crabb DW. Peroxisome proliferator-activated receptor alpha (PPARalpha) agonist treatment reverses PPARalpha dysfunction and abnormalities in hepatic lipid metabolism in ethanol-fed mice.
J Biol Chem 2003;278:7997-8004. PMID:
10.1074/jbc.M302140200.
100. Dey A, Cederbaum AI. Alcohol and oxidative liver injury.
Hepatology 2006;43:S63-74. PMID:
10.1002/hep.20957. PMID:
16447273.

102. You M, Crabb DW. Molecular mechanisms of alcoholic fatty liver: role of sterol regulatory element-binding proteins.
Alcohol 2004a;34:39-43. PMID:
10.1016/j.alcohol.2004.07.004. PMID:
15670664.

103. You M, Crabb DW. Recent advances in alcoholic liver disease II. Minireview: molecular mechanisms of alcoholic fatty liver.
Am J Physiol Gastrointest Liver Physiol 2004b;287:G1-6. PMID:
10.1152/ajpgi.00056.2004. PMID:
15194557.

104. Chen YH, Yang CM, Chang SP, Hu ML. C/EBP beta and C/EBP delta expression is elevated in the early phase of ethanol-induced hepatosteatosis in mice.
Acta Pharmacol Sin 2009;30:1138-43. PMID:
10.1038/aps.2009.109. PMID:
19617893.


105. Mohiuddin I, Chai H, Lin PH, Lumsden AB, Yao Q, Chen C. Nitrotyrosine and chlorotyrosine: clinical significance and biological functions in the vascular system.
J Surg Res 2006;133:143-9. PMID:
10.1016/j.jss.2005.10.008. PMID:
16360172.

106. Rogers CQ, Ajmo JM, You M. Adiponectin and alcoholic fatty liver disease.
IUBMB Life 2008;60:790-7. PMID:
10.1002/iub.124. PMID:
18709650.

107. Leung TM, Lu Y, Yan W, Morón-Concepción JA, Ward SC, Ge X, Conde de la Rosa L, Nieto N. Argininosuccinate synthase conditions the response to acute and chronic ethanol-induced liver injury in mice.
Hepatology 2012;55:1596-609. PMID:
10.1002/hep.25543. PMID:
22213272.

108. Zhou Z, Wang L, Song Z, Saari JT, McClain CJ, Kang YJ. Zinc supplementation prevents alcoholic liver injury in mice through attenuation of oxidative stress.
Am J Pathol 2005;166:1681-90. PMID:
10.1016/S0002-9440(10)62478-9. PMID:
15920153.

109. Dubinina EE, Dadali VA. Role of 4-hydroxy-trans-2-nonenal in cell functions.
Biochemistry (Mosc) 2010;75:1069-87. PMID:
10.1134/S0006297910090014. PMID:
21077827.


111. Galligan JJ, Smathers RL, Shearn CT, Fritz KS, Backos DS, Jiang H, Franklin CC, Orlicky DJ, Maclean KN, Petersen DR. Oxidative Stress and the ER Stress Response in a Murine Model for Early-Stage Alcoholic Liver Disease.
J Toxicol 2012;207594:PMID:
10.1155/2012/207594.